
a National Department Of Health, Waigani, Papua New Guinea.
b World Health Organization Papua New Guinea, Port Moresby, Papua New Guinea
c School of Public Health and Community Medicine, Faculty of Medicine, University of New South Wales, Sydney, New South Wales, Australia.
Correspondence to Boris Pavlin (e-mail: pavlinb@wpro.who.int).
To cite this article:
Dagina R et al. Event-based surveillance in Papua New Guinea: strengthening an International Health Regulations (2005) core capacity. Western Pacific Surveillance and Response Journal, 2013, 4 (3):19–25. doi:10.5365/wpsar.2013.4.2.001
Under the International Health Regulations (2005), Member States are required to develop capacity in event-based surveillance (EBS). The Papua New Guinea National Department of Health established an EBS system during the influenza pandemic in August 2009. We review its performance from August 2009 to November 2012, sharing lessons that may be useful to other low-resource public health practitioners working in surveillance.
We examined the EBS system’s event reporting, event verification and response. Characteristics examined included type of event, source of information, timeliness, nature of response and outcome.
Sixty-one records were identified. The median delay between onset of the event and date of reporting was 10 days. The largest proportion of reports (39%) came from Provincial Health Offices, followed by direct reports from clinical staff (25%) and reports in the media (11%). Most (84%) of the events were substantiated to be true public health events, and 56% were investigated by the Provincial Health Office alone. A confirmed or probable etiology could not be determined in 69% of true events.
EBS is a simple strategy that forms a cornerstone of public health surveillance and response particularly in low-resource settings such as Papua New Guinea. There is a need to reinforce reporting pathways, improve timeliness of reporting, expand sources of information, improve feedback and improve diagnostic support capacity. For it to be successful, EBS should be closely tied to response.
Event-based surveillance (EBS) is defined as “the organized and rapid capture of information about events that are a potential risk to public health.”1 Rumours or other ad hoc reports are transmitted through formal and informal channels such as media, health workers, community leaders and nongovernmental organizations, and assessments on the risk these events pose to public health enable a timely, effective and measured response.
Under the Asia Pacific Strategy for Emerging Diseases,2 and to meet requirements of the International Health Regulations or IHR (2005),3 the Papua New Guinea National Department of Health (NDOH) established an EBS system in August 2009 during the influenza A(H1N1) pandemic. One surveillance and one administrative officer received reports about potential public health events from community members, health workers, embassies and daily media. The EBS system was established to complement the existing indicator-based surveillance systems operating in provincial hospitals, which, due to poor timeliness, were inappropriate for the early detection of public health events. This paper reviews the performance of the EBS system from 2009 to 2012, sharing lessons that may be useful to other low-resource public countries in initiating or improving their surveillance systems.
A simple Microsoft Excel database captures the nature of events (e.g. chemical, infectious, food safety); location; dates of events, reports and follow-ups; sources of reporting; verification status; and responses. The database is maintained by an EBS Coordinator within the Command Centre of the Communicable Diseases Surveillance and Emergency Response (CDS&ER) Unit of NDOH.
The system receives ad hoc reports from any source, including health workers, nongovernmental organizations, embassies, media and the general public. Reports are received at CDS&ER or the World Health Organization (WHO) and are channelled to the EBS Coordinator. Active surveillance through review of the two major national newspapers is also conducted. However, by routing data directly from the ground level to the national level, the system bypasses established reporting channels, i.e. from local/district to provincial to national levels.
Using a structured questionnaire (Figure 1), the EBS Coordinator verifies events reported from non-health sources by contacting the nearest health authorities or provincial health offices (PHOs) who are responsible for disease surveillance and control. Information about the presenting syndrome, place and date of occurrence and number of cases and deaths due to the syndrome are collected. The EBS Coordinator also provides guidance to provincial health authorities about investigation and response measures. A log of all verification, assessment and follow-up activities is maintained in the EBS database.

The legal mandate for outbreak investigation and response lies primarily with PHO. In specific circumstances (e.g. events associated with a particular health facility or mining enterprise), investigations may be initiated directly by affected parties. Support from higher levels (e.g. NDOH, WHO and/or other partners) occurs only upon request from local authorities. The EBS Coordinator follows up periodically with the relevant PHO to obtain reports about the local response.
All events investigated through the EBS system are reported back to stakeholders (e.g. provincial health authorities, hospital management) through a weekly National Surveillance Bulletin.
We conducted a descriptive analysis of the line-list of events captured by EBS from August 2009 to November 2012; calculated the proportion of events that were verified, responded to and laboratory confirmed; and assessed the timeliness of the system by calculating the interval between occurrence and reporting to the system and between reporting and verification of events.
There were 61 unique records in the EBS system. From August to December 2009, 10 events were recorded; 22 events were recorded in 2010; five in 2011; and 17 in 2012 (Table 1). Additionally, there were seven events recorded for which no dates were available. There was no clear pattern to the time of event reporting (data not shown).
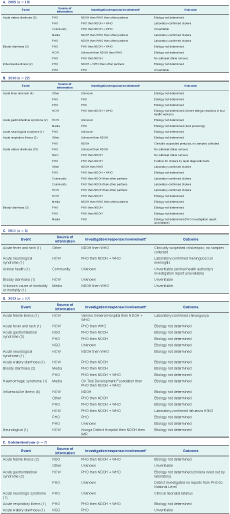
HCW – Health care worker; IMR – Papua New Guinea Institute of Medical Research; NDOH – National Department of Health; NGO – Nongovernmental organization; PHO – Provincial Health Office; WHO – World Health Organization.
* Investigation and response includes both remote verification/advice and onsite field investigation.
The most common reports (n = 16) were of acute watery diarrhoea, followed by bloody diarrhoea (n = 9), influenza-like illness (n = 8), acute gastrointestinal syndromes (n = 7) and acute fever and rash (n = 6). Other events included neurological syndrome (n = 5), unspecified acute febrile illness (n = 3), acute respiratory illness not classified as influenza-like illness (n = 3), a haemorrhagic syndrome, an animal die-off and an unknown cause of death.
Among 36 events for which both data were available, the median delay between event onset and date of reporting was 10 days (range= 0–109 days). Ten events (28%) took more than 30 days to report. Fourteen of the 23 reports not coming from health care workers or public health authorities had both dates listed; of these, all but one were verified with the relevant local health authorities on the same day they were received.
The largest number of reports (n = 24) came from PHOs followed by direct reports from clinical health care workers (n = 15), media (n = 7), other sources (n = 6), nongovernmental organizations (n = 4) and the community (n = 4). The reports were widely geographically distributed (data not shown).
Most events (n = 34) were investigated directly by the PHO. A minority involved either onsite or remote assistance from NDOH, with or without support from WHO in Papua New Guinea and/or the regional office in Manila, Philippines or other development partners. A few events involved investigations conducted solely by a third party (e.g. the reporting hospital or a mining company).
Most events (n = 51) were substantiated to be true public health events. Only three events were discarded as false reports; an additional six could not be verified, and one record did not report final outcome.
Among the true events, confirmed or probable etiologies were identified in 16, and in the remaining 35, the etiology could not be determined.
EBS is a simple-to-use strategy that forms a cornerstone of public health surveillance and response, particularly in low-resource settings such as Papua New Guinea. It is adaptable to a wide variety of public health events and settings, especially rare events and those occurring in populations that do not access the formal health care system (e.g large segments of the 87% rural population in Papua New Guinea).4 For it to be successful, EBS should be closely tied to response; formalization of EBS through the use of assessment tools and response tracking, as described in WHO’s Guide to Establishing Event-based Surveillance,1 facilitates this response.
The single largest source of reports to the EBS system was the PHO, which is expected given the requirement for PHOs to report serious public health events to the national government. However, that the majority of reports were received through other sources, such as health care workers and the media, points to a need to reinforce to partners that their first point of contact should be the PHO, in line with their authority to implement public health measures.
The EBS system is fully flexible for any type of public health event; the system successfully identified a chemical event and a nutritional emergency. The incorporation of new reporting sources is relatively easily accomplished, although feedback to distant sites may be a challenge.
The cost of the system, although not formally evaluated, appears exceptionally low, requiring two part-time staff members, and incurring little more cost than that of the phone calls and electricity involved. The great cost, of course, comes later in the need to respond to the many true outbreaks that are detected by the system. One logistical barrier is the frequent lack of phone credit on the part of informants (even Provincial Disease Control Officers who are directly responsible for outbreak investigations), which could be remedied by employing a toll-free reporting number; this would likely improve sensitivity and acceptability, as it would obviate the need for reporters to incur individual costs by reporting, although it would increase the cost of the system at the national level.
Formalizing the system beyond simply receiving rumour reports (i.e. by using standardized forms and logging all reports) has several benefits. These include improved accountability, since, once a report is logged, it must be pursued until it is investigated or dismissed; a more consistent approach to assessing reports; the ability to evaluate the relative contribution of disparate reporting sources; and others. In our opinion, these benefits far outweigh the additional burden of collecting EBS data systematically.
It is equally crucial to regularly disseminate EBS performance characteristics and findings back to reporters and other stakeholders. This is currently done through a weekly National Surveillance Bulletin, although its reach is currently limited to those stakeholders who can receive e-mail. Increasing the reach of the bulletins, including through broadcasting findings over the well-established radio network for health posts, is being explored.
One of the challenges of the current system is the bypassing of provincial authorities of reports made directly from nongovernmental organizations or the public to the national government. This has required awareness-raising/training of provincial authorities on the benefits of an additional source of surveillance information.
The objective of EBS is to identify events early to enable rapid verification and response if the event poses a risk to public health. In Papua New Guinea, there is certainly room for improvement as public health events were identified after a median delay of 10 days. Nevertheless, given that indicator-based data are often subject to a delay of three months or more, EBS is timelier. Far more concerning is the fact that 28% of EBS events took more than 30 days to be investigated. After such a delay the opportunity for control is largely lost, and limited resources are wasted on mounting largely fruitless responses.
Another challenge of the system is in reaching the majority rural population, who, by virtue of their remoteness, may not be aware of benefits and mechanisms of reporting events or who simply cannot do so. For this reason it may be useful to consider strengthening EBS in high-risk settings first. This may include raising awareness of EBS among large employers in remote settings with a high degree of international mobility, such as those in the extractive industries or logging workers who are at the interface of potential sylvatic zoonotic disease transmission events.
The EBS system in Papua New Guinea could further be improved by systematically collecting information from media sources, both traditional and social; by being more responsive to the media, for example by publishing articles in response to media stories; and proactively reaching out to health reporters to improve story accuracy. While EBS is more sensitive than the routine indicator-based surveillance system, given the high specificity of the EBS reports (only 5% of reports are discarded as non-events), there is room to improve the sensitivity of the system by casting a wider net.
It is reassuring that most responses were initiated by the PHO in the respective province, especially as most PHOs are quite limited in the extent to which they can conduct field investigations. For example, most Provincial Disease Control Officers do not have reliable access to a computer or a vehicle, and most have never formally been trained in epidemiologic principles. There is an urgent need to train these individuals for them to fulfil their mandates. Therefore, NDOH and WHO are now incorporating EBS training into all surveillance training and resource materials such as the Papua New Guinea Field Epidemiology Training Programme and the recently updated Papua New Guinea Outbreak Manual.
As evidenced by the huge proportion of events for which an etiology could not be determined, improvements in diagnostic capacity are urgently needed. This is primarily an issue of sample collection and transport, rather than an issue of actual analysis, as described for the 2010 national cholera outbreak.5
EBS is a critical asset for Papua New Guinea’s public health surveillance. Through this system, Papua New Guinea has successfully met virtually all of the IHR requirements related to EBS; the only area requiring further work is direct outreach to communities to increase reporting. The EBS system has effectively identified a large number of urgent public health events and instigated prompt responses to those events. Elements of the system such as feedback and the link to laboratory confirmation need to be strengthened for the system to function to its full potential.
None declared.
None.