Assessment of the risk posed to Singapore by the emergence of artemisinin-resistant malaria in the Greater Mekong Subregion
Risk Assessment
Emma Xuxiao Zhang,a Jean-Marc Chavatte,b Cherie See Xin Yi,a Charlene Tow,a Wong Jia Ying,a Kamran Khan,c,d Olivia Seen Huey Oh,a Sarah Ngeet Mei Chin,a Khong Wei Xin,a Zubaidah Said,a Lyn James,a Jeffery Cutter,a Marc Hoa and Jeannie Su Hui Teya
a Ministry of Health, Singapore.
b National Public Health Laboratory, National Centre for Infectious Diseases, Singapore.
c Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, Canada.
d Department of Medicine, Division of Infectious Diseases, University of Toronto, Toronto, Canada.
Correspondence to Emma Xuxiao Zhang (email: emma_zhang@moh.gov.sg).
To cite this article:
Zhang EX, Chavatte JM, Yi CSX, Tow C, Ying WJ, Khan K, et al. Assessment of the risk posed to Singapore by the emergence of artemisinin-resistant malaria in the Greater Mekong Subregion. Western Pac Surveill Response J. 2019 May;10(2). doi:10.5365/wpsar.2018.9.2.011
Abstract
Objective: To assess the public health risk to Singapore posed by the emergence of artemisinin-resistant (ART-R) malaria in the Greater Mekong Subregion (GMS).
Methods: We assessed the likelihood of importation of drug-resistant malaria into Singapore and the impact on public health of its subsequent secondary spread in Singapore. Literature on the epidemiology and contextual factors associated with ART-R malaria was reviewed. The epidemiology of malaria cases in Singapore was analysed. The vulnerability and receptivity of Singapore were examined, including the connectivity with countries reporting ART-R malaria, as well as the preparedness of Singaporean health authorities. Sources of information include international journals, World Health Organization guidelines, data from the Singapore Ministry of Health and National Public Health Laboratory of the National Centre for Infectious Diseases, and the International Air Transport Association.
Results: The importation of ART-R malaria into Singapore is possible given the close proximity and significant travel volume between Singapore and the GMS countries reporting artemisinin resistance. Singapore’s vulnerability is further enhanced by the presence of foreign workers from neighbouring endemic countries. Nonetheless, the overall likelihood of such an event is low based on the rarity and decreasing trend of imported malaria incidence.
With the presence of Anopheles vectors in Singapore, imported cases of drug-resistant malaria could cause secondary transmission. Nevertheless, the risk of sustained spread is likely to be mitigated by the comprehensive surveillance and control system in place for both infected vectors and human cases.
Discussion: This risk assessment highlights the need for a continued high degree of vigilance of ART-R malaria locally and globally to minimize the risk and public health impact of drug-resistant malaria in Singapore.
Objective
Despite remarkable global progress in the fight against malaria since 2010, growing resistance to antimalarial drugs remains the biggest challenge on the path towards malaria elimination.1 To date, drug resistance has been recorded in Plasmodium falciparum, P. vivax and P. malariae.2,3 The development of resistance by P. falciparum to nearly all antimalarial drugs, including current first-line treatments artemisinin and its derivatives, has become an issue of utmost concern. The Greater Mekong Subregion (GMS), which comprises Cambodia, the Lao People’s Democratic Republic, Myanmar, Thailand, Viet Nam and Yunnan Province of China, has long been the epicentre of antimalarial drug resistance.4 The first cases of artemisinin resistance were reported in Cambodia in 2008.5 Since then, artemisinin resistance has been observed in other countries in the GMS and in neighbouring India.5,6 Concomitantly, variable levels of resistance to the partner drugs used in artemisinin-based combination therapies (ACTs) have been reported.4
Singapore is a globally connected city-state in South-East Asia with high travel connectivity with many countries in the world, including those in the GMS, due to its position as a travel and trade hub. Although Singapore has been declared malaria-free by the World Health Organization (WHO) since 1982, Singapore is at risk of importation of emerging diseases including artemisinin-resistant (ART-R) malaria. In view of the emergence of resistance across the GMS and the spread beyond its borders, we carried out an analysis to assess the risk of importation and secondary spread of ART-R malaria infection in Singapore.
Methods
The risk of importation of drug-resistant malaria into Singapore and the public health impact of its subsequent secondary spread in Singapore were assessed following WHO guidance on the risk assessment of acute public health events.7 The process of risk assessment included relevant literature review, epidemiological analysis of malaria cases in Singapore, analysis of the air travel volume between Singapore and countries reporting artemisinin resistance, an assessment of the vulnerability and receptivity of Singapore, and the preparedness of Singaporean health authorities to a potential (case/introduction/outbreak) of ART-R malaria. The risk assessment was conducted by four public health officers specializing in public health surveillance, epidemiology and risk analysis of infectious diseases. Their findings were reviewed by a broader group of experts from the Singapore Ministry of Health (MOH) in the areas of public health, laboratory medicine, epidemiology, infectious diseases, risk communication and emergency preparedness and response.
The epidemiology of malaria cases in Singapore was analysed based on information released by the MOH.8 A qualitative review of the public health measures taken by Singapore in response to the emerging threat was conducted based on information released by the MOH and the Singapore National Environment Agency (NEA). The volume of travellers on commercial flights originating from countries with ART-R malaria and with final destinations in Singapore in 2017 was analysed using data from the International Air Transport Association (IATA) in Singapore. The IATA data are reported monthly and contain anonymized, itinerary-level passenger volumes. The data capture an estimated 90% of the world’s air traffic, with the remainder being imputed using market intelligence. Full itineraries of the travellers have been used, including the initial airport of embarkation, final destination and any connecting flights. IATA data have been used previously to inform risk assessments of the spread of pathogens of epidemic potential.9 Among the imported P. falciparum cases, the monitoring of artemisinin resistance based on the Kelch 13 (K13) gene was performed by the Malaria Reference Centre from the National Public Health Laboratory (MRC-NPHL) by polymerase chain reaction (PCR) amplification and sequencing according to the protocol of Ariey et al.10
Risk Assessment
Hazard assessment
Malaria is caused by Plasmodium parasites that are transmitted to people through the bites of female Anopheles mosquitoes with infectious sporozoites of malaria parasites.11 Five Plasmodium species cause malaria in humans: P. falciparum, P. vivax, P. malariae, P. ovale and P. knowlesi. P. falciparum is responsible for most malaria-related deaths globally and is the most prevalent malaria parasite in Africa, while P. vivax is the dominant malaria parasite in most countries outside of sub-Saharan Africa including those in South-East Asia.1 The first symptoms of malaria—fever, headache, chills and vomiting—usually appear between 10 to 15 days after a bite from a vector mosquito with infectious sporozoites of malaria parasites. Without prompt diagnosis and treatment, P. falciparum malaria can rapidly progress to severe illness and death.11 Currently, the most effective treatments are ACTs.12,13
Drug resistance has been one of the greatest challenges in fighting malaria. Resistance usually develops progressively, from the initial delay of parasite clearance in a few locations to the gradual expansion of geographic range and increase in prevalence, eventually leading to treatment failure. Of the various antimalarial drugs available, chloroquine was the agent of choice for many years because of its safety, efficacy and affordability. However, since its first detection along the border of Cambodia and Thailand in 1957, resistance of P. falciparum to chloroquine has spread to almost everywhere that P. falciparum exists.14 P. falciparum has also developed resistance to nearly all other available antimalarial drugs, including sulfadoxine, pyrimethamine, amodiaquine, mefloquine, piperaquine, atovaquone and an increasing frequency of reported quinine resistance in several regions.15
The first clinical evidence of artemisinin resistance originated in western Cambodia in 2008; however, further retrospective studies of molecular markers have indicated that artemisinin resistance likely emerged before 2001 and the widespread usage of ACTs.5,16,17 The extensive and often suboptimal usage of monotherapies as well as the genetic background of parasites in the GMS were thought to have contributed to the development of resistance.18 Since then, emergence of resistance to artemisinin and ACT partner drugs such as piperaquine have been reported in other areas in the GMS.19,20 Nevertheless, most patients with delayed parasite clearance can still be cured using ACTs as long as the partner drug remains effective; there is no evidence that higher levels of artemisinin resistance (full resistance) have emerged.4
Exposure assessment
Reports of imported malaria infections in Singapore
In Singapore, malaria was the most common vector-borne disease in the early 20th century, resulting in substantial morbidity and mortality.21 With strengthened epidemiological and vector control measures, Singapore was certified malaria-free by WHO in November 1982. Since 2010, the annual incidence of malaria has continued to decrease from 3.7 cases per 100 000 population in 2010 to 0.7 cases per 100 000 population in 2017. Incidence has been maintained below 1 per 100 000 population in recent years. The number of imported malaria cases steadily decreased from 187 cases in 2010 to 39 cases in 2017.
Among the 290 cases of malaria reported in Singapore between 2013 and 2017, 289 (99.7%) were imported cases, of whom 141 (49%) were work-permit or employment pass holders. The majority of imported cases were from South-East Asia (16%), Africa (16%) and India (62%). Among the cases imported from South-East Asia, most were from Indonesia and Malaysia, which accounted for 8% and 4% of cases, respectively. Most of the cases of malaria reported in Singapore between 2013 and 2017 were caused by P. vivax (70%) followed by P. falciparum (22%).
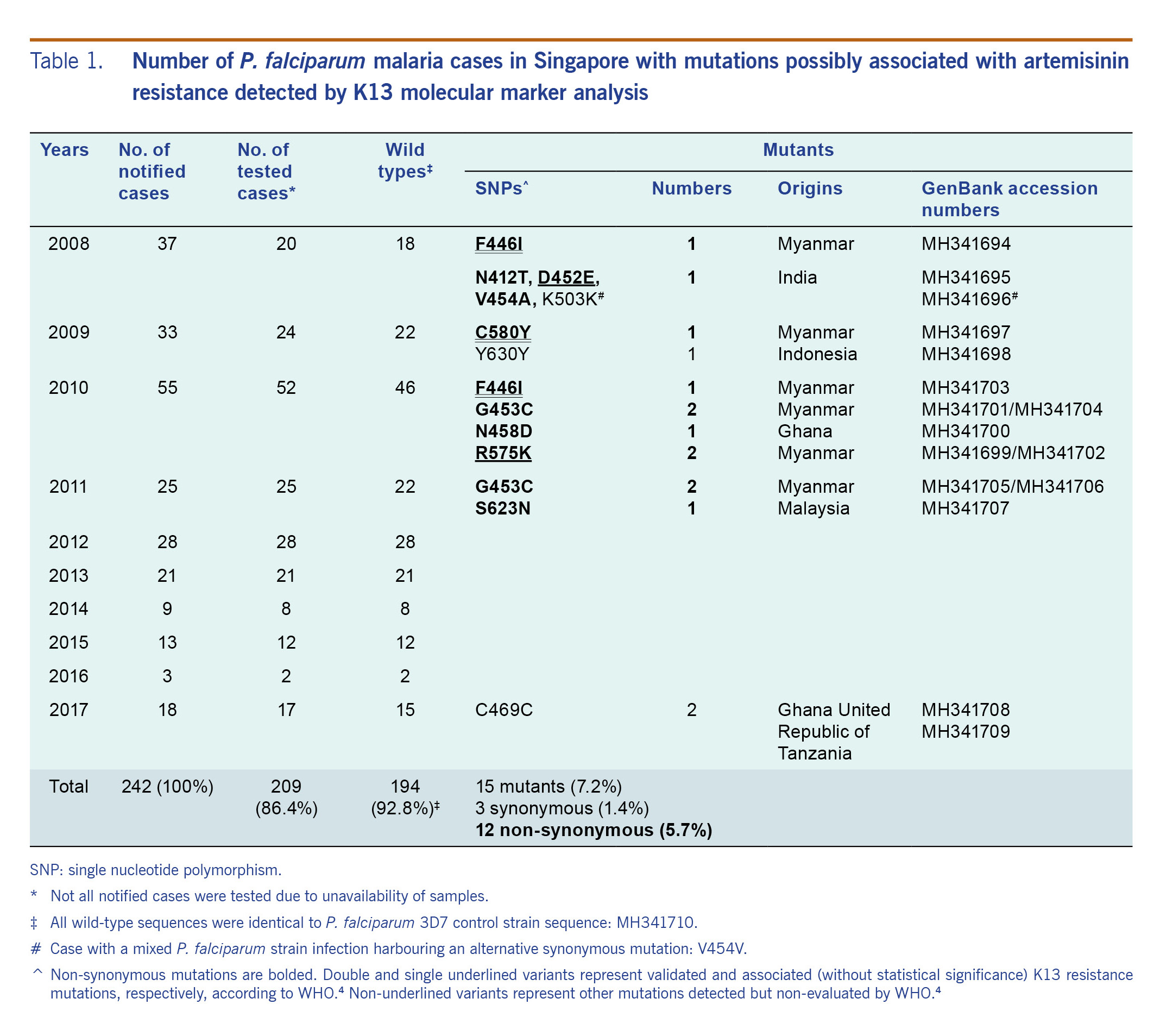
In a retrospective survey from 2008 to 2017, 12 out of 209 (5.7%) P. falciparum cases tested had mutations possibly associated with artemisinin resistance (Table 1). Of the 12 cases, three cases had validated K13 resistance mutations while two cases had candidate K13 resistance mutations classified by WHO.4 However, none experienced treatment failure and all recovered without complications.
Table 1. Number of P. falciparum malaria cases in Singapore with mutations possibly associated with artemisinin resistance detected by K13 molecular marker analysis
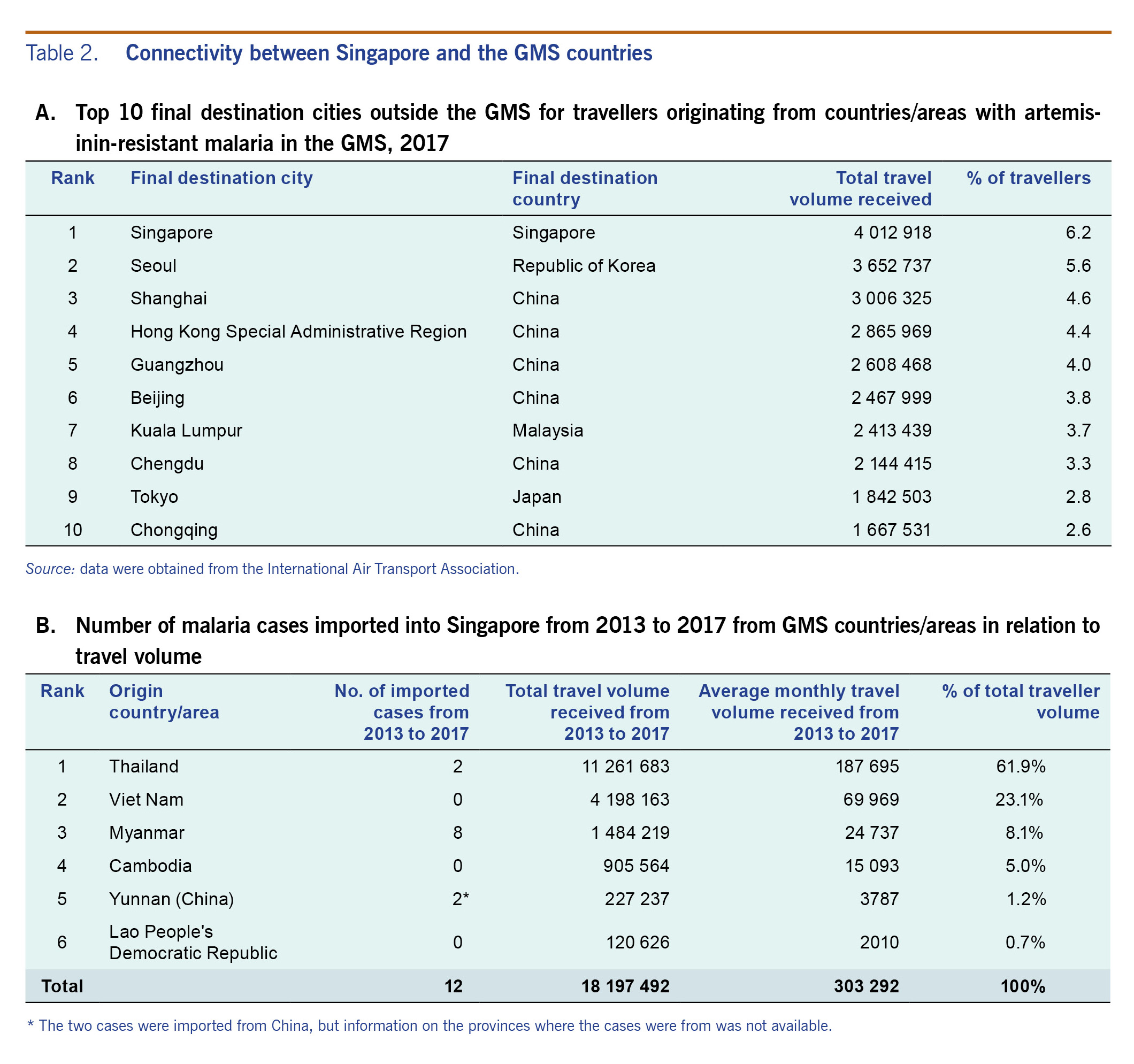
Travel volume from the GMS to Singapore
Among cities outside the GMS, Singapore receives the highest number of travellers from the GMS (Table 2A). From 2013 to 2017, there was an average of more than 303 000 travellers each month from the GMS to Singapore (Table 2B). Thailand accounted for the highest number of travellers followed by Viet Nam and Myanmar. More than 15 000 monthly travellers to Singapore came from Cambodia where artemisinin resistance was first detected. Despite being a major international transportation hub with high connectivity to the GMS, importation of malaria into Singapore appears to be rare (Table 2B).
Table 2. Connectivity between Singapore and the GMS countries
Context assessment
Vector distribution
Singapore remains vulnerable and receptive to the reintroduction of malaria and the introduction of drug-resistant malaria due to the presence of Anopheles vectors. Among the over 400 species of Anopheles mosquitoes discovered globally to date, about 70 species are potential vectors of malaria.22 In Singapore, the two most common Anopheles species are Anopheles epiroticus and Anopheles sinensis.23 Anopheles epiroticus, Anopheles maculatus and Anopheles letifer, were reported to be involved in malaria outbreaks in Singapore in the 1960s and 1970s, while Anopheles sinensis was implicated in the 2009 outbreak.24,25
Preparedness and response in Singapore
Malaria surveillance and control in Singapore is under the purview of two public health agencies: the NEA, which undertakes the surveillance and control of Anopheles mosquitoes, and the Singapore MOH, which is responsible for case surveillance and epidemiological investigation. Vector control remains the cornerstone for controlling mosquito-borne diseases, including malaria. NEA has put in place an integrated vector surveillance and control programme comprising environmental management and source reduction.26 NEA has also identified specific malaria receptive areas for regular Anopheles surveillance and control.27 Malaria is a legally notifiable disease under the Infectious Disease Act and all medical practitioners and laboratories are required to notify the MOH within 24 hours of diagnosis.28 The MOH then investigates all cases of malaria to determine if transmission is likely to be locally acquired or imported and assess whether any clusters are present. The MRC-NPHL has the capability to detect a large panel of molecular markers associated with antimalarial drug resistance, including the WHO-recommended K13 gene (as a marker of artemisinin resistance) and several genes associated with partner drug resistance.
To address the issue of imported malaria cases among foreign workers, Singapore implemented compulsory screening for malaria for foreign workers in 1997 as part of the pre-employment medical examinations. Among Singapore residents diagnosed with imported malaria infections from 2012 to 2016, more than 90% did not observe adequate preventive measures such as taking chemoprophylaxis before overseas travel.29 Such behaviours could be due to the lack of risk perception associated with travel, especially within Asia, and the lack of awareness of travel medicine among travellers.29
Past outbreaks of malaria in the event of an imported case
Although imported cases continue to pose challenges for malaria control, the chances of resumption of endemic transmission are small as elimination tends to be a stable state.30 Singapore has maintained its malaria-free status31 since 1982. Between 1983 and 2009, 32 outbreaks involving 225 cases were reported, and the majority of the cases were imported through foreign workers with relapsing P. vivax malaria.26 Further transmissions from these occasional outbreaks were promptly curbed by aggressive preventive and remedial actions, including extensive vector surveillance and control measures; early case detection through blood and fever surveys in malaria receptive areas; and risk communication to medical practitioners as well as health education for the public.26 No outbreaks have been reported since 2010.
Measures taken by GMS countries
To prevent global spread of artemisinin resistance, containment efforts have been initiated in the GMS. In 2015, WHO launched the Strategy for malaria elimination in the Greater Mekong Subregion (2015–2030), which was endorsed by all GMS countries.31 All GMS countries have begun to implement national malaria elimination strategies that have resulted in a significant reduction in malaria cases and death; the surveillance of the efficacy of antimalarial drugs has led to prompt updating of malaria treatment policies in most GMS countries.1
Risk characterization
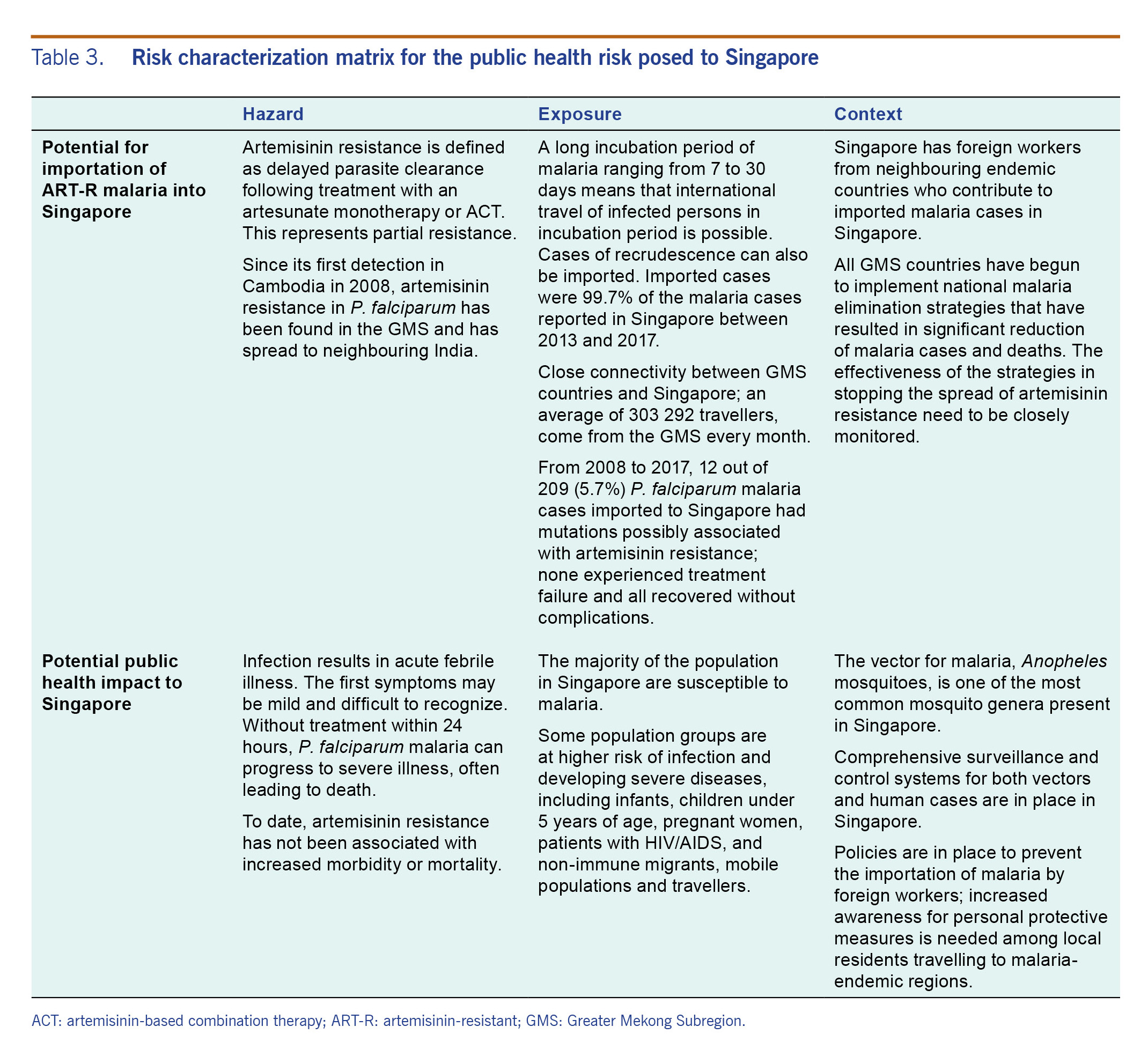
The risk imposed to Singapore by the emergence of ART-R malaria was characterized using the information collected; key factors were considered to assess the likelihood of importation of cases into Singapore and the impact on public health (Table 3).
Table 3. Risk characterization matrix for the public health risk posed to Singapore
The risk characterization of likely based on the likelihood of importation and the according minimal consequence suggest that the overall risk of ART-R malaria to Singapore is low. The importation of a case of ART-R malaria into Singapore is possible given the close proximity and significant travel volume between Singapore and the GMS countries reporting artemisinin resistance. Singapore’s vulnerability is further enhanced by the presence of foreign workers from neighbouring endemic countries. Nonetheless, the overall likelihood of importation is considered low based on the rarity and the decreasing trend of imported malaria incidence over the past few years.
With the presence of Anopheles vectors in Singapore, imported cases of ART-R malaria can cause secondary transmission. The risk of sustained spread is likely to be mitigated by the comprehensive surveillance and control system in place for both infected vectors and human cases as observed in the past local outbreaks of malaria initiated by imported cases.
Discussion
Singapore is the top destination for travellers from the GMS. Among the imported P. falciparum cases in Singapore, 5.8% had genetic mutations that may confer resistance to artemisinin. The presence of competent local vectors, the high volume of travel from regions with ART-R malaria, and the presence of foreign workers from neighbouring endemic countries make it possible that drug-resistant malaria could be imported and introduced to Singapore. To reduce the risk of Singapore residents acquiring malaria infections overseas, pre-travel health education, particularly by travel agents, the media and health-care providers, can increase awareness of the risk of contracting malaria overseas so that personal preventive measures can be taken.
Secondary spread following an imported case is also possible. However, any spread is not likely to be sustained. Malaria has not re-established itself as an endemic disease in Singapore despite local outbreaks since it was declared malaria-free in 1982. The Singapore MOH and NEA have implemented comprehensive malaria surveillance and control programmes to detect cases and curb the transmission of local outbreaks.
The risk assessment has some limitations. The assessment is based on limited data as the number of imported cases of malaria in Singapore is small. As the risk characterization was defined by the epidemiological and contextual knowledge available currently, conclusions could change as new information emerges. Ongoing studies on genetic mutations, particularly their underlying molecular and cellular mechanisms and their phenotypic manifestations in resistance, could provide a better understanding of an epidemic and facilitate the design of surveillance and control measures. Identification of new molecular markers and improvements in laboratory capability continues to impact disease surveillance as illustrated by the significant progress in global surveillance of artemisinin resistance expedited by the discovery of the molecular marker K13.12 Risk assessment will also change as new treatment options become available. Even though an assessment of the risks posed by resistance to partner drugs in the ACTs is out of scope for this paper, we recognize the risk of such resistance and the importance of monitoring all molecular markers of antimalarial-drug resistance. Analysis is currently under way to test molecular markers for partner drugs and assess potential variations. In addition, artemisinin resistance has also been observed in non-GMS countries, including countries in Africa, although the occurrence is very rare.4 The risk of importation of ART-R malaria from these non-GMS countries is not discussed in this paper because of low connectivity of Singapore with these countries. Nevertheless, it warrants our close monitoring of the development of global situations.
In conclusion, in view of the emergence of ART-R malaria in the GMS and its geographical expansion, this risk assessment highlights the need for a high degree of vigilance over the local and global situation to be maintained to minimize the risk and severity of the public health threat of ART-R malaria to Singapore.
Acknowledgements
We are grateful to Dr Derrick Heng (Group Director of the Public Health Group), Dr Vernon Lee (Director of the Communicable Diseases Division), and Dr Raymond Lin (Head of the National Public Health Laboratory) of Singapore Ministry of Health for their valuable advice. We would also like to thank Mr Matthew German and Mr Deepit Bhatia of Bluedot Inc. for feedback on the manuscript and helpful discussions.
Funding
None.
Conflicts of interest
None.
References
-
World malaria report 2018. Geneva: World Health Organization; 2018 (https://www.who.int/malaria/publications/world-malaria-report-2018/en/, accessed 27 November 2018).
-
White NJ, Pukrittayakamee S, Hien TT, Faiz MA, Mokuolu OA, Dondorp AM. Malaria. Lancet. 2014 Feb 22;383(9918):723–35.
doi:10.1016/S0140-6736(13)60024-0
pmid:23953767
-
Worldwide Antimalarial Resistance Network [website]. Oxford: Worldwide Antimalarial Resistance Network; 2017 (https://www.wwarn.org/, accessed 29 December 2017).
-
Status report on artemisinin and artemisinin-based combination therapy resistance. Geneva: World Health Organization; 2018 (https://apps.who.int/iris/bitstream/handle/10665/274362/WHO-CDS-GMP-2018.18-eng.pdf?ua=1, accessed 28 November 2018).
-
Noedl H, Se Y, Schaecher K, Smith BL, Socheat D, Fukuda MM; Artemisinin Resistance in Cambodia 1 (ARC1) Study Consortium. Evidence of artemisinin-resistant malaria in western Cambodia. N Engl J Med. 2008 Dec 11;359(24):2619–20.
doi:10.1056/NEJMc0805011
pmid:19064625
-
Das S, Saha B, Hati AK, Roy S. Evidence of artemisinin-resistant Plasmodium falciparum malaria in eastern India. N Engl J Med. 2018 Nov 15;379(20):1962–4.
doi:10.1056/NEJMc1713777
pmid:30428283
-
Rapid risk assessment of acute public health events. Geneva: World Health Organization; 2012 (https://www.who.int/csr/resources/publications/HSE_GAR_ARO_2012_1/en/, accessed 30 April 2018).
-
Resources & statistics. In: Singapore Ministry of Health [website]. Singapore: Singapore Ministry of Health; 2019 (https://www.moh.gov.sg/resources-statistics, accessed 11 April 2019).
-
Brent SE, Watts A, Cetron M, German M, Kraemer MU, Bogoch II, et al. International travel between global urban centres vulnerable to yellow fever transmission. Bull World Health Organ. 2018 May 1;96(5):343–354B.
doi:10.2471/BLT.17.205658
pmid:29875519
-
Ariey F, Witkowski B, Amaratunga C, Beghain J, Langlois AC, Khim N, et al. A molecular marker of artemisinin-resistant Plasmodium falciparum malaria. Nature. 2014 Jan 2;505(7481):50–5.
doi:10.1038/nature12876
pmid:24352242
-
Fact sheet on malaria. Geneva: World Health Organization; 2018 (https://www.who.int/en/news-room/fact-sheets/detail/malaria, accessed 30 April 2018).
-
Guidelines for the treatment of malaria, 3rd edition. Geneva: World Health Organization; 2015 (https://apps.who.int/iris/bitstream/10665/162441/1/9789241549127_eng.pdf?ua=1&ua=1, accessed 30 April 2018).
-
Artemisinin and artemisinin-based combination therapy resistance. Geneva: World Health Organization; 2017 (https://apps.who.int/iris/bitstream/10665/255213/1/WHO-HTM-GMP-2017.9-eng.pdf?ua=1, accessed 30 April 2018).
-
Payne D. Spread of chloroquine resistance in Plasmodium falciparum. Parasitol Today. 1987 Aug;3(8):241–6.
doi:10.1016/0169-4758(87)90147-5
pmid:15462966
-
Thu AM, Phyo AP, Landier J, Parker DM, Nosten FH. Combating multidrug-resistant Plasmodium falciparum malaria. FEBS J. 2017 Aug;284(16):2569–78.
doi:10.1111/febs.14127
pmid:28580606
-
Dondorp AM, Nosten F, Yi P, Das D, Phyo AP, Tarning J, et al. Artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2009 Jul 30;361(5):455–67.
doi:10.1056/NEJMoa0808859
pmid:19641202
-
Amato R, Pearson RD, Almagro-Garcia J, Amaratunga C, Lim P, Suon S, et al. Origins of the current outbreak of multidrug-resistant malaria in southeast Asia: a retrospective genetic study. Lancet Infect Dis. 2018 03;18(3):337–45.
doi:10.1016/S1473-3099(18)30068-9
pmid:29398391
-
Dondorp AM, Fairhurst RM, Slutsker L, Macarthur JR, Breman JG, Guerin PJ, et al. The threat of artemisinin-resistant malaria. N Engl J Med. 2011 Sep 22;365(12):1073–5.
doi:10.1056/NEJMp1108322
pmid:21992120
-
Imwong M, Suwannasin K, Kunasol C, Sutawong K, Mayxay M, Rekol H, et al. The spread of artemisinin-resistant Plasmodium falciparum in the Greater Mekong subregion: a molecular epidemiology observational study. Lancet Infect Dis. 2017 05;17(5):491–7.
doi:10.1016/S1473-3099(17)30048-8
pmid:28161569
-
Woodrow CJ, White NJ. The clinical impact of artemisinin resistance in Southeast Asia and the potential for future spread. FEMS Microbiol Rev. 2017 Jan;41(1):34–48.
doi:10.1093/femsre/fuw037
pmid:27613271
-
Goh KT. Eradication of malaria from Singapore. Singapore Med J. 1983 Oct;24(5):255–68.
pmid:6669988
-
Sinka ME, Bangs MJ, Manguin S, Rubio-Palis Y, Chareonviriyaphap T, Coetzee M, et al. A global map of dominant malaria vectors. Parasit Vectors. 2012 Apr 4;5(1):69.
doi:10.1186/1756-3305-5-69
pmid:22475528
-
Not all mosquitoes transmit dengue. Singapore: The National Environmental Agency; 2018 (https://www.nea.gov.sg/corporate-functions/resources/research/wolbachia-aedes-mosquito-suppression-strategy/not-all-mosquitoes-transmit-dengue, accessed 9 July 2018).
-
Ng LC, Lee KS, Tan CH, Ooi PL, Lam-Phua SG, Lin R, et al. Entomologic and molecular investigation into Plasmodium vivax transmission in Singapore, 2009. Malar J. 2010 Oct 29;9(1):305.
doi:10.1186/1475-2875-9-305
pmid:21029478
-
Pang SC, Andolina C, Malleret B, Christensen PR, Lam-Phua SG, Razak MABA, et al. Singapore’s Anopheles sinensis Form A is susceptible to Plasmodium vivax isolates from the western Thailand-Myanmar border. Malar J. 2017 Nov 16;16(1):465.
doi:10.1186/s12936-017-2114-3
pmid:29145859
-
Lee YCA, Tang CS, Ang LW, Han HK, James L, Goh KT. Epidemiological characteristics of imported and locally-acquired malaria in Singapore. Ann Acad Med Singapore. 2009 Oct;38(10):840–9.
pmid:19890574
-
Malaria receptive areas in Singapore. Singapore: The National Environmental Agency; 2018 (https://data.gov.sg/dataset/malaria-receptive-areas, accessed 9 July 2018).
-
List of infectious diseases legally notifiable under the Infectious Diseases Act. Singapore: Singapore Ministry of Health; 2019 (https://www.moh.gov.sg/docs/librariesprovider5/default-document-library/list-of-infectious-diseases-legally-notifiable-under-the-ida.pdf, accessed 11 April 2019).
-
Lin YJ, Badaruddin H, Ooi SPL. Epidemiology of malaria in Singapore, 2008–2015. Epidemiological News Bulletin. 2016;42(2):49–54.
-
Smith DL, Cohen JM, Chiyaka C, Johnston G, Gething PW, Gosling R, et al. A sticky situation: the unexpected stability of malaria elimination. Philos Trans R Soc Lond B Biol Sci. 2013 Jun 24;368(1623):20120145.
doi:10.1098/rstb.2012.0145
pmid:23798693
-
Strategy for malaria elimination in the GMS (2015–2030). Geneva: World Health Organization; 2015 (https://iris.wpro.who.int/bitstream/handle/10665.1/10945/9789290617181_eng.pdf, accessed 11 April 2019).