a Special Preventive Programme, Department of Health, Hong Kong Special Administrative Region, China.
Correspondence to Ada Wai-Chi Lin (email: adalinwc@gmail.com).
To cite this article:
Surveillance and response of hepatitis B virus in Hong Kong Special Administrative Region, 1988–2014. Western Pacific Surveillance and Response Journal, 2016, 7(1):24–27. doi:10.5365/wpsar.2015.6.3.003
The World Health Organization (WHO) Western Pacific Region with an estimated 160 million chronic hepatitis B virus (HBV) carriers in 2007 bears a significant burden of HBV-related mortality and morbidity.1 Most Member States in the region have an estimated chronic HBV infection proportion of more than 8% in their adult population, which is the highest worldwide.2 The WHO Regional Office for the Western Pacific published the first Regional Plan for Hepatitis B Control1 in January 2003. This plan is updated periodically with a consistent ultimate goal of achieving a chronic HBV infection rate of less than 1% in the region.
Viral hepatitis is a statutorily notifiable disease in Hong Kong Special Administrative Region (SAR). The Central Notification Office of the Department of Health receives notifications with pre-defined case definitions.3 In July 2011, Hong Kong SAR was verified by the WHO Regional Office for the Western Pacific as having successfully achieved the goal of hepatitis B control.4
Liver cancer was the third leading cause of cancer death in Hong Kong SAR in 2012,5 and evidence showed that 75–80% of liver cancer cases were related to chronic HBV infection.6 This report reviews the surveillance data of HBV infections in Hong Kong SAR from 1988 to 2014 and discusses the responses and existing gaps to achieve the WHO goal in the local context.
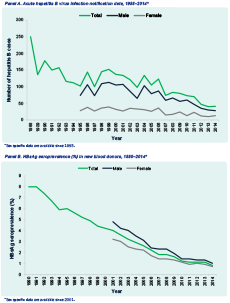
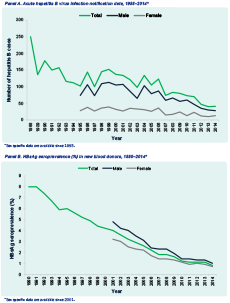
Viral hepatitis has been a statutorily notifiable disease since 1974 in Hong Kong SAR. Collation and analysis of surveillance data obtained from various sources were compiled in the annual reports of surveillance of viral hepatitis by the Department of Health, Hong Kong SAR.7 We extracted HBV-specific data from the reports, including acute HBV infection notification data for the period 1988 to 2014 and hepatitis B surface antigen (HBsAg) seroprevalence data from 1990 to 2014.
Data on acute HBV infections were obtained from the Department of Health Central Notification Office that centralizes communicable diseases notifications and monitoring in Hong Kong SAR. A case of acute hepatitis B is defined as a person having clinically compatible acute hepatitis illness with laboratory confirmation of hepatitis B core antibody immunoglobulin M positive result.3
HBsAg seroprevalence data were obtained from various sources, including Hong Kong Red Cross Blood Transfusion Service; Family Planning Association of Hong Kong SAR, a nongovernmental organization providing screening for clients attending pre-marital and pre-pregnancy check-ups; Family Health Service; Public Health Laboratory Service; Tuberculosis and Chest Service; and HIV/AIDS Service of the Department of Health. Data were collected annually in 1990–2014. Data from Tuberculosis and Chest Service only covered data from March to May in 1990–2014.
Annual acute hepatitis B notification and HBsAg seroprevalence data were compared for trends. Data were stratified by sex for analysis. HBsAg seroprevalence data were also analysed among specific groups, including at-risk groups that are defined as groups with risk of blood-borne or sexual transmission of hepatitis B. All analysis was done by Excel (Microsoft Excel 2010, Redmond, USA).
A downward trend was observed for both acute and chronic HBV infections. The reported number of acute HBV infections decreased steadily from 250 cases in 1988 to 41 cases in 2014 (Figure 1). For chronic HBV infections in new blood donors the rate dropped from 8.0% in 1990 to 0.8% in 2014 (1.0% for males and 0.7% for females). Among adults, the decreasing trend was also observed, albeit less prominently, in antenatal women (11.3% in 1990 to 6.2% in 2014), pre-marital/pre-pregnancy screening clients (9.6% in 1990 to 5.5% in 2014) and police officers (6.1% in 1996 to 2.6% in 2014). Based on the available data, the HBsAg seroprevalence was 9.5% and 7.5% in people living with HIV in 2000 and 2014, respectively and was 6.8% and 7.2% in female sex workers in 1995 and 2011, respectively.
The results show that Hong Kong SAR evolved from a region of high-intermediate to intermediate-low hepatitis B endemicity from 1988 to 2014. The decrease is probably due to concerted preventive efforts applied since the late 1980s, including community-based vaccination, public awareness programmes and measures such as antiviral subsidies and specialist referral for treatment, institution-based infection control to prevent occupational exposure and methadone treatment programmes for drug users to prevent infections of blood-borne pathogens.
Adequate vaccination policies in the past decades contributed significantly to reducing HBV infections. A local prospective study demonstrated the long-term protective effect of neonatal HBV vaccination for up to 30 years in high-risk infants borne to HBsAg-positive mothers.8 Since 1988, the universal neonatal hepatitis B immunization programme has continued to record high birth dose coverage rates (99.1–99.6% in 2008 to 2013). For neonates of HBsAg-positive mothers, hepatitis B immunoglobulin was also given at birth to further reduce the risk of perinatal infection. The percentage of children aged 2 to 5 years who completed three doses of HBV vaccine exceeded 98.8% in 2012.7 A supplementary hepatitis B vaccination programme for primary school students was introduced in 1998. From 2004 to 2014, the coverage of three-dose HBV vaccination among the students each year was 99% on average.7 HBV immunization programmes were also in place for prioritized adult populations including health-care workers since 1983. High vaccine coverage provides sufficient individual and herd immunity against HBV infections.
Currently, the major burden of HBV infections in Hong Kong SAR lies in the adult population (aged 30 or above) who did not benefit from the universal neonatal hepatitis B immunization programme. While the risk of developing a chronic infection when contracting the virus in adulthood is generally low,9 it is a public health priority to address the burden of morbidity and mortality from HBV infections among adults. At-risk groups, including health-care workers, injecting drug users, patients undergoing dialysis, and household contacts and sexual partners of persons with chronic hepatitis B, should be screened and referred to medical care. Currently, serological testing for HBV markers is implemented only in some of these targeted populations. Efforts should be extended for screening and linkage to medical care for the at-risk adult population who have not been screened and vaccinated. Meanwhile, territory-wide information of chronic HBV infection is essential for disease control. Robust data provided by different stakeholders and the potential use of mathematical modelling for disease and treatment burden estimation should be explored.
This study used only secondary data for analysis; the quality of some of the data from private agencies could not be controlled. In addition, there were missing data on specific groups that might have hindered the comparison, and more in-depth analysis could not be performed on these aggregated data. However, using official data from the government for analysis ensured data quality.
Hong Kong SAR has evolved from a region of high-intermediate to one with intermediate-low hepatitis B endemicity in the past decades. Adequate vaccination policies are likely to contribute to reducing HBV infections. Specific interventions should be conducted targeting the at-risk groups. More robust territory-wide HBV infection data should be collected and analysed for disease control.
None declared.
None.
The authors would like to thank all colleagues and partners of the Department of Health, the Hospital Authority and the academic and private sector for their collaboration and contributions to hepatitis B surveillance and control in Hong Kong SAR.