a Office of the WHO Representative in the Philippines, Sta Cruz, Manila, Philippines.
b Mayor Alfred’s Social Action Health Service Unit (MASA), Tacloban City, Philippines.
Correspondence to Allison Gocotano (email: gocotanoa@who.int or allisongocotano@gmail.com).
To cite this article:
Czaicki AE et al. Is my drinking a problem? A community-based alcohol intervention programme post-Haiyan in Tacloban City. Western Pacific Surveillance and Response Journal, 2015, 6(Suppl 1):96–101. doi:10.5365/wpsar.2015.6.2.HYN_016
Problem: Evidence on alcohol use following disasters is scarce. After Typhoon Haiyan in the Philippines we wanted to determine whether there were alcohol-related problems among the disaster survivors and to strengthen the appropriate local health service support in Tacloban City.
Context: Tacloban City is a highly urbanized city that was one of the areas worst hit by Typhoon Haiyan. Prior to Haiyan there was very little support for people with alcohol problems, and the rehabilitation facility was located about 40 km away.
Action: A pilot community-based alcohol intervention programme was conducted that included: assessment of the extent of alcohol problems in the community and health-care workers baseline knowledge and skills; training of health-care workers on primary care alcohol intervention provision; and community outreach with post-training supervision.
Outcome: The alcohol screening found 26 (22%) of those attending healthcare facilities would benefit from some form of alcohol intervention. Health-care workers knowledge on basic alcohol intervention was low. This was strengthened during the training, and at outreach clinics the trained health-care workers were able to identify people with alcohol problems and provide them with treatment plans.
Lessons learnt: We learnt that there was a problem with alcohol in Tacloban City and that it was possible to run an alcohol intervention programme in the community using minimal resources. Addressing alcohol-related issues in the community is an important public health intervention. While there is a need for policies and guidelines at the national level, a community-based intervention is possible to establish with referral mechanism to specialized care. Training modules for such programs can be further developed and institutionalized.
Alcohol is widely used around the world in socio-cultural and traditional means; excessive use as a coping mechanism for emotional stress also occurs.1 Alcohol has been causally related to at least 60 medical conditions with 4% of the global burden of disease attributable to alcohol.2 Total alcohol consumption in the Philippines has been projected to increase from 5.6 litres of pure alcohol per capita consumption in 2015 to 6.5 litres in 2025, which suggests there will be an increase in demand for alcohol-related health services in the future.3
Among survivors of Hurricane Katrina, alcohol and drug consumption was associated with greater post-traumatic stress disorder symptoms.4 However, it has been shown that alcohol use disorders post-disaster were more likely a recurrence or continuation of pre-existing problems as opposed to new incidents.5,6 This increase in alcohol use is caused by accumulated traumatic events and stressors and that contribution of point-in-time mass traumatic events subsides over time. A more recent study among Norwegian survivors of the 2004 South-East Asia tsunami showed that disaster exposure was associated with both self-perceived increases and decreases in drinking.7 Overall, evidence in post-disaster alcohol use needs to be strengthened.
In the Philippines, a country that experiences many disasters, there is no national policy or action plan for alcohol problems or community-level support from the government for persons with alcohol problems. There are no alcohol restrictions set on alcohol outlet density, availability at public events, serving intoxicated persons or sales at petrol stations and no legally binding regulations on alcohol advertising and sponsorship. There is the Ad Standard Council, a self-regulating mechanism of the local advertising body that, in their 2012 guidebook, prescribed the inclusion of the words “drink responsibly” in alcohol product advertisements.8 There are health warning labels on alcohol containers and a national maximum legal blood alcohol concentration of 0.05% when driving a vehicle; however, there is no national monitoring system in place and no effective means of enforcement.3 The Anti-Drunk and Drugged Driving Act, passed only in 2013, focuses on penalizing people driving under the influence of alcohol but does not cover any provision for rehabilitation.
As part of the response to Typhoon Haiyan in November 2013, the Mental Health Gap Action Programme (mhGAP) was conducted by the World Health Organization (WHO) and Department of Health (DOH) and other key stakeholders.9 As part of this mental health initiative, the WHO Representative Office in the Philippines piloted a community-based alcohol intervention programme in Tacloban City, one of the areas worst hit by Typhoon Haiyan, to determine the extent of alcohol-related problems and to train local health staff to provide community-based alcohol intervention services.
Tacloban City is a highly urbanized city with a population of 221 174.10 Prior to Haiyan, interventions for harmful alcohol use were not part of the local health services and there were no community groups (e.g. Alcoholics Anonymous) for people to seek help.
The Comprehensive Dangerous Drugs Act of 2002 mandated that DOH manage the Drug Abuse Treatment and Rehabilitation Centers nationwide,11 but these were intended for drug dependence only. Neither the law nor the manual for rehabilitation centres included rehabilitation for alcohol problems. This is despite four of the accredited centres including alcohol rehabilitation as part of their institution’s name.12 These centres provide facility-based interventions with outpatient services for follow-up. Mental health services are not available at the primary care level in the entire country, and this is only now being addressed through lobbying of the Philippine Mental Health Act of 2014.13
The DOH-accredited rehabilitation facility within Region 8 is located about 40 km outside Tacloban City.12 Access to this facility is difficult for people with low incomes because of this distance from the city and also because clearances from village, police and regional trial court are required for admission.14 There have been no patients treated for alcohol disorders at this facility, likely due to inaccessibility and the non-functioning referral system from primary care. There are tertiary-level hospitals within Tacloban City and one has a psychiatry department that can provide medical support for detoxification. However, as the main referral hospital catering to the entire region, it is always full of patients, understaffed and lacks resources.
We were unable to find any report of a community-based intervention for alcohol rehabilitation in the Philippines. This is despite experiences in other lower- to middle-income countries that have shown that medical treatment and detoxification of mild to moderate alcohol withdrawal can be safely managed in outpatient settings under the supervision of community nurses supported by local medical practitioners.15 Treatment research suggests that early intervention at the primary care level can be both feasible and effective for heavy drinkers who do not have evidence of severe alcohol dependence, medical or psychiatric complications.2
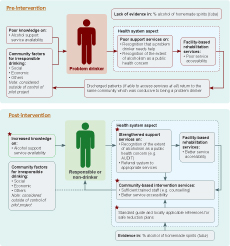
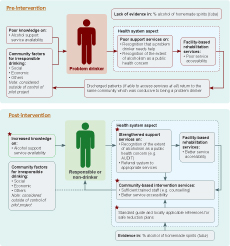
The pilot community-based alcohol intervention programme had three components: assessment, training and outreach. Assessment measured baseline alcohol-related problems within Tacloban City and the knowledge and skills of local health staff regarding alcohol and safe and effective treatment options. Training taught a team of local health workers to provide alcohol intervention services. Outreach involved supervising local health workers to screen and provide interventions to patients with alcohol problems. Underpinning this pilot was a conceptual framework which highlighted the opportunities for implementing community-based alcohol interventions (Figure 1). Homemade spirits that had no accurate alcohol percentage was a barrier in designing safe reduction plans.
The initial assessment was conducted in three urban sites located near the city centre: the Mayor Alfred Social Action Health Service Unit (MASA), Sagkahan Health Center and Tacloban City Hall. MASA is the main health care centre in the city and provides community outreach services to surrounding villages. Nurses regularly travel to hard-to-reach locations to provide basic health services.
We used two tools for the assessment: (1) the CAGE questionnaire, which is a screening tool with four yes/no questions;16 and (2) the Alcohol Use Disorders Identification Test (AUDIT), a more sensitive tool for measuring alcohol dependence and harmful drinking patterns which comprises 10 questions and was recommended in mhGAP.17 A score of 7 and above on the AUDIT tool was considered indicative of harmful alcohol use requiring some intervention.18,19
The two questionnaires were translated into local languages by local health staff and project consultants. Nursing staff administered the tools at all three sites to adults seeking medical treatment, their companions and people in public waiting areas. Between 2 and 6 February 2015, CAGE was initially administered to adults (≥ 18 years) who provided verbal consent. However, the results showed that 166 (70%) of respondents required an alcohol intervention which seemed unrealistic. Therefore, the more sensitive AUDIT tool was used and, after orientation of staff, was administered at the same sites from 12 to 18 February 2015.
A training programme was developed based on the alcohol-related problems, challenges and experiences observed by health-care staff and community members. It was open to participants with varied technical health backgrounds including community volunteers, social workers and medical doctors. The training, delivered mostly through lectures, consisted of alcohol unit conversion and low-risk drinking guidelines,20 the effects of alcohol on health, Foetal Alcohol Spectrum Disorder, mental health, alcohol dependency and screening tools (AUDIT). Training for the health-care staff included medications used to treat alcohol disorders.
Pre-topic assessments were conducted to determine existing knowledge before the training; for example, participants were provided with a human body outline and were asked to draw which organs were affected by alcohol.
There was a separate training session for nursing staff from the alcohol unit in the treatment centre and MASA that focused on designing safe reduction plans (the gradual decrease in alcohol consumption), unit calculation and alcohol withdrawal management plans, indicators of alcohol dependency and the use and interpretation of the alcohol screening tools. The training was delivered by an international consultant supported by a national psychiatrist. Participants were encouraged to begin routinely screening their patients for alcohol problems.
One of the most affected villages by Haiyan on the outskirts of Tacloban City was chosen for outreach. The newly trained MASA staff were to administer alcohol screening services during their usual health services under the supervision of the trainers. The clinic was open to the whole community.
The CAGE assessment of 239 people resulted in 31%, 56% and 13% of respondents being rated as having a low, medium or high risk of alcohol problems, respectively (Table 1). From the AUDIT, 22% (26 of 117) of respondents, six females and 20 males (8% and 47%, respectively), had a high risk and required some alcohol intervention (Table 1). Respondents were from 39 of the 138 villages in Tacloban City and were more likely to be members of the urban poor with little or no access to alcohol intervention services within their practical means.
* AUDIT scores by intervention adapted in this pilot: low risk, 0–2; medium risk, 3–6 (needs alcohol education); high risk, ≥ 7 (7–15, needs simple advice; 16–19, plus brief counselling and continued monitoring; and 20–40, referral to specialist for diagnostic evaluation and treatment). Sixty-seven respondents answered 0–2.
AUDIT, alcohol use disorders identification test; CAGE, a screening tool with four yes/no questions.
The assessment of the knowledge and skills of local health staff regarding alcohol and safe and effective treatment options showed that they did not know how to approach a patient with suspicion of alcohol problems, and had no knowledge on the use of screening tools or on the relationship of alcohol to mental health. Overall, there was poor baseline knowledge by health staff on effective and safe treatment methods, which they attributed to the fact that such services were not provided. Health staff also showed a lack of knowledge regarding alcohol units and low-risk drinking levels and minimal baseline information on the specific harms of alcohol.
When local health workers were asked what they would do when faced with a person who had a problem with alcohol, the common response was that the patient would leave the clinic without any kind of treatment, advice or information.
Three separate training sessions were conducted for a total of 52 participants who included doctors, nurses, social workers and village health staff. The participants came from MASA, the City Social Welfare and Development Office and the DOH-Dulag, Leyte Treatment & Rehabilitation Center. Participants with a clinical background received more technical lectures.
The outreach clinic identified 20 people requiring alcohol services using the AUDIT. These patients were offered counselling, had safe reduction plans designed for them and follow-up support with referral to specialized care when needed. Feedback from those who agreed to undergo assessment revealed that they had not previously sought help and were unaware that help of any kind was available.
Many lessons were learnt from this pilot. We provided the first evidence that alcohol problems do exist in Tacloban City and that treatment for people with alcohol disorders, especially the poor, does not. Local health-care workers and other village staff were somewhat aware of the problems caused by alcohol but were ill-equipped to give appropriate and effective support to individuals who needed it. Patients who did recognize that they had a problem and wanted help reported they did not know where to seek it. This baseline situation was improved through our community-based programme, which was feasible to setup with minimal resources. Brief intervention and motivational interviewing through community visits and targeted client home visits provided a valuable initiative for supporting people with alcohol problems in the community.
We do not know if the level of alcohol use reported in this study is indicative of the level before Typhoon Haiyan or if it was an increase. The effect of disaster exposure on self-perceived changes in alcohol consumption has been observed, yet no significant association between disaster exposure and current alcohol use has been established.7 We also do not know if the level is higher in Tacloban City than in the rest of Region 8. Regardless of the applicability of the results to other settings, the levels of alcohol use in Tacloban City found by this study are concerning enough to need further public health intervention.
Addressing alcohol-related issues in the community is a valuable public health intervention both post-disaster and in non-emergency times. The increased capacity of health professionals to assess and support people with alcohol problems can reduce alcohol-related harm. We have shown that community-based supportive services for alcohol were needed in Tacloban City and were achieved with minimal resources, including training on screening methods, designing alcohol reduction plans and building networks for specialized care. For this pilot, we only needed the commitment and willingness from local health staff; the continuation of the programme required no additional budget allowance. The assessment of patients for alcohol problems and subsequent treatment plans were integrated into the services already offered to the community by the local health nurses. Perhaps the main barriers were the lack of evidence demonstrating that problem drinking is indeed an issue in the local community and the lack of technical capacity to address problem drinking at the primary level.
There were several limitations to this pilot project. The initial assessment used convenience sampling, and the participation refusal rate was not recorded. There was no structured evaluation for the trained health professionals or the patients. However, informal feedback from two of the trained participants indicated they had increased their knowledge, confidence and ability to make a difference to those who are seeking help and are willing to change. Furthermore, local health authorities have verified the service implemented in this pilot has continued as part of the regular package of services with referral to specialized care when needed along with integration with the social service office. MASA has also incorporated the alcohol screening questions as part of their Healthy Lifestyle clinic day, which is held every Thursday. All identified high-risk patients are offered alcohol intervention support. Four months after the pilot, the programme had helped treat three alcohol-dependent people, and clients from this health programme are now automatically referred for livelihood support and other family improvement opportunities.
It is important that efforts are made to establish locally applicable, national-level, low risk drinking guidelines so the public and professionals are guided accordingly. There is also a need to conduct research on the impact of homemade spirits in the community. We recommend determining if the magnitude of alcohol problems in Tacloban City is the same elsewhere in the Philippines and institutionalizing community-based alcohol intervention programmes as well as developing local referral systems for alcohol intervention services.
None declared.
None.
We thank all the trainers, trainees and nurses that participated and continues to implement thos community-based alcohol intervention programme.
The authors would also like to thank the WHO Representative Office in the Philippines-Mental Health and Psychosocial Support Team, with special mention to Dr Katryn Beluso who supported the preparation and successful implementation of this pilot programme.