a Office of the WHO Representative in the Philippines, Sta Cruz, Manila, Philippines.
b National TB Control Programme, Infectious Diseases Office, Department of Health, Sta Cruz, Manila, Philippines.
Correspondence to Woojin Lew (email: leww@who.int).
To cite this article:
Lew W et al. Restarting the tuberculosis programme post-Haiyan. Western Pacific Surveillance and Response Journal, 2015, 6(Suppl 1):91–95. doi:10.5365/wpsar.2015.6.2.HYN_009
Problem: Typhoon Haiyan damaged or destroyed health infrastructure, equipment and services essential to the Philippine National Tuberculosis Programme (NTP), and it had to be re-established in the affected areas in Regions 6, 7 and 8. Continuing treatment and restoring diagnostic capacity were also challenging.
Context: The Philippines has one of the highest tuberculosis (TB) burdens in the world. At the time of Typhoon Haiyan, there were an estimated 26 600 TB cases on treatment at directly observed treatment, short-course (DOTS) centres and 356 multidrug-resistant TB cases registered at programmatic management of drug-resistant TB (PMDT) sites. As TB was not included in the Philippines early-warning post-disaster surveillance system, tracking TB patients was difficult after Haiyan.
Actions and outcomes: Immediately following Haiyan, each aspect of the NTP was assessed to determine the extent of damage. TB patients were traced and services restored. We created maps showing the location of temporary TB diagnostic and treatment services, which hastened referrals. We provided new laboratory equipment, training and rapid testing capabilities in the affected regions. All TB services in the affected areas (473 DOTS, 490 TB microscopy and six PMDT facilities) were restored just two months after Haiyan.
Lessons learnt: Key lessons learnt from the NTP experience following Tyhoon Haiyan were: (1) the importance of having an electronic TB registry (database); (2) the need to include TB in the post-disaster surveillance system; (3) clear guidelines for TB control in disasters; and (4) the importance of coordination with all partners.
The Philippines is an incredibly disaster-prone country,1 and as a result, the government and its citizens have experience in disaster preparedness, response and recovery. However, tuberculosis (TB) control in a disaster has been somewhat neglected. In the areas where facilities, records and equipment were damaged by Typhoon Haiyan, the Philippine National TB Control Programme (NTP) had to be re-established quickly.
The Philippines has the eighth highest TB burden in the world and the second highest in the World Health Organization (WHO) Western Pacific Region.2 In 2013, the estimated incidence of TB in the Philippines was 292 cases per 100 000 population.2 Improvements to case detection, treatment success, and access to services especially in difficult geographic and socioeconomic settings have been observed.3 When Typhoon Haiyan hit the central Philippines on 8 November 2013, there were approximately 26 600 TB patients and 356 multidrug-resistant TB cases (MDR-TB) under treatment in the affected area.4
Since the overall disaster response focused on surgical intervention and preventing disease outbreaks, TB did not receive much attention in the initial response. TB was not included in the Surveillance in Post Extreme Emergencies and Disasters (SPEED) system, an early warning surveillance system that becomes operational following disasters, which uses a syndromic approach to identify consultation trends in health facilities and evacuation centres.5 Post-Haiyan, the highest priority for the NTP was to ensure that existing TB patients continued to receive treatment, which posed two significant challenges: (1) locating all existing TB patients; and (2) facilitating full treatment for these patients. Another priority was to restore diagnostic capability as soon as possible to detect undiagnosed TB cases in the community. We report on the actions taken and lessons learnt from the re-establishment of the NTP in these affected areas.
In the days immediately following Typhoon Haiyan, regional and provincial TB coordinators from affected areas in Regions 6, 7 and 8, health emergency management staff, and other partners conducted an assessment of the 473 directly observed treatment, short-course (DOTS) facilities, 490 TB microscopy centres and six programmatic management of drug-resistant TB (PMDT) facilities. They assessed the level of damage to the facilities, the availability of human resources, the status of microscopy services, the adequacy of drug supply and the condition of records and reports. These assessments were repeated until all facilities were deemed functional at eight weeks post-Haiyan (Table 1).
* Based on data provided by regional coordinators.
DOTS, directly observed treatment, short-course; TB, tuberculosis; PMDT, programmatic management of drug-resistant TB.
The NTP and WHO prepared guidelines for the provision of TB services in areas affected by Haiyan6 and these were distributed to the three most affected Regional Health Offices (RHOs) and their health partners on 2 December 2013. The guidelines outlined how to conduct a rapid assessment to determine the current status and availability of diagnostic equipment, human resources, drug supply, facilities, records and reports. It instructed the RHOs on how to re-establish DOTS services to ensure all existing TB patients resumed treatment as soon as possible. Lastly, it provided guidance for the management of presumptive TB and new TB cases including MDR-TB; improving TB laboratory services; and logistics management, supervision and monitoring.6
By 9 December 2013, a month after Haiyan, using the results from the initial assessments, maps were created that detailed the location of the operational DOTS and PMDT diagnostic and treatment services (Figures 1a and 1b). These maps were the basis of a referral system and allowed local and foreign medical teams on the ground to know where to refer TB patients and suspected TB cases. Contact details of key staff and operational centres through the Health Cluster network were also collected in the assessments and included maps that facilitated rapid referrals.
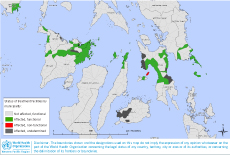
Note: Green colour indicates that DOTS facilities in municipalities were physically damaged, but TB treatment services were available. Red colour indicates that TB treatment service was not available. Black colour indicates that information on functionality of TB services was not available yet.
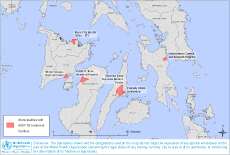
Note: Out of six MDR-TB centres, Schistomiasis Control and Research Hospital in Leyte province was completely damaged but restored its MDR-TB diagnosis and treatment in a tent within four weeks after the typhoon.
DOTS, directly observed treatment, short-course; MDR-T B: multidrug-resistant tuberculosis.
Typhoon Haiyan had impacted the diagnostic capability in the affected areas. Approximately two thirds of the health infrastructure in the affected regions were not functional one week after the typhoon hit (Table 1). To strengthen laboratory capacity in diagnosing TB, including rifampicin (RIF)-resistant TB, Hayian-affected regions were prioritized for delivery of Xpert® MTB/RIF assay machines (Xpert; Cepheid, USA). These machines were considered suitable as they have a rapid diagnostic turnaround time of two hours and do not require a sophisticated laboratory infrastructure, a special facility or condition to be installed.7 Two Xpert machines belonging to the National TB Reference Laboratory were initially deployed to the Eastern Visayas Regional Medical Center on 27 January 2014 with eight additional Xpert units shipped to affected areas in February 2014. There were no Xpert machines in the affected areas before Haiyan.
Following the needs assessments and an official request from the Department of Health in May 2014, WHO procured 50 Light Emitting Diode (LED) microscopes that could operate on either electric or solar power. These were distributed through the NTP to prioritized health units in the affected areas.
In the initial stages of the response, microscopes were shared and medical technologists rotated among neighbouring health units. Suspected TB cases or their sputum samples were transferred to health facilities that had microscopy services. WHO supported two trainings on Xpert testing in February and March 2014 where 22 laboratory technicians received hands-on training. An additional five trainings on LED microscopic examination were also conducted for 60 microscopists in May and June 2014.
The necessary equipment required to detect and manage TB cases: anti-TB drugs; forms (treatment card, identification card, NTP laboratory register, TB register); laboratory supplies (sputum cups, reagents); equipment (microscopes and Xpert MTB/RIF machines); and policies were packed in a single container and distributed through NTP.
Within two months of the typhoon, TB DOTS services were completely restored to pre-typhoon levels (Table 1). This collaborative effort showed the extraordinary dedication of NTP staff. Most of the case notes and records were lost, but the health staff recalled the names of many of their TB patients, and follow-up could take place through village health workers, relatives and family members of patients. One of the completely destroyed Regional Health Units, a health facility which serviced a population of approximately 21 000, continued to provide TB treatment services on a daily basis in a tent.
In many instances, the high rate of resumption of TB DOTS services was due to patients returning to DOTS facilities once they opened. Health workers recorded the number of people who had received treatment before the typhoon, who had received treatment after the typhoon and those who were reported as having died or were missing. The less affected health facilities were able to trace close to 100% of their TB patients. As well as this, there were 7944 suspected TB cases that underwent smear microscopy tests and 1101 new smear positive cases on treatment by March 2014.8
One PMDT site was completely destroyed; however, it became fully functional in four weeks using tents once the roads to the facility were cleared. Second-line TB drugs, particularly levofloxacin, were supplied through PMDT and Philippines Business of Social Progress or Global Fund channels. Fortunately, the records of patents with MDR-TB were stored in an electronic database, and all 356 MDR-TB patients were located. In the five undamaged PMDT facilities, all MDR-TB patients were back on treatment within 2–16 days post-Haiyan; it took almost 12 weeks for the severely damaged PMDT centre to get all patients back on treatment. By mid-February 2014, all 356 MDR-TB patients were back on treatment.
Although it took time to restore normal TB drug delivery and distribution, no drug shortage was experienced in the affected areas. It is the usual practice in the Philippines for the TB DOTS facility to store and gradually distribute a six-month drug supply for new TB cases. After Haiyan, those stored medicines were shared to cover the temporary shortage of medicines until normal supplies resumed.
This paper has some limitations. First, an accurate number of TB patients registered at DOTS facilities in Regions 6, 7 and 8 before Haiyan was unavailable as paper-based TB records were missing or damaged in most affected areas. Not being able to compare the number of cases pre- and post-Haiyan limited the assessment of the NTP response at DOTS facilities for tracking and getting patients back on treatment. Treatment outcomes such as treatment success rates and default rates were also unavailable for pre-Haiyan; therefore, the negative impact of the typhoon on treatment compliance could not be assessed. The number of new TB cases detected could also not be compared between pre- and post-typhoon, which limits the assessment of case-finding activities at the facility level that could help indicate the level of NTP recovery.
The first lesson learnt from Typhoon Haiyan was the importance of an electronic TB registry of DOTS patients, not just the MDR-TB patients. Not having baseline data for comparisons pre- and post-Haiyan limited our ability to assess the response; relying on paper-based records was not feasible in this disaster-prone region. Adding TB to SPEED should be considered to assist in finding TB patients for referral to the NTP as soon as possible. Clear policies and guidelines for TB control in disasters are needed for better preparation, response and recovery for future disasters,8 including specific monitoring and evaluation indicators that will allow for comparisons to be made pre- and post-disaster. It is necessary to coordinate and collaborate with all partners involved in the response to more effectively and efficiently meet the needs of TB patients in affected areas.
None declared.
None.
We thank the regional and provincial TB coordinators and other partner organizations that assisted in re-establishing TB programmes.