a Field Epidemiology Training Program, Epidemiology Bureau, Department of Health, San Lazaro Compound, Sta Cruz, Manila, Philippines.
b Department of Health, San Lazaro Compound, Sta Cruz, Manila, Philippines.
c Emerging Disease Surveillance and Response Unit, Division of Health Security and Emergencies, World Health Organization Regional Office for the Western Pacific, Manila, Philippines.
Correspondence to Imelda Deveraturda (email: deveraturdamel@gmail.com).
To cite this article:
Deveraturda I et al. Chelonitoxism outbreak: Sorsogon, Philippines, October 2014. Western Pacific Surveillance and Response Journal, 2015, 6(2):90–91. doi:10.5365/wpsar.2015.6.1.021
Recently, a chelonitoxism (turtle poisoning) outbreak in Arteche, Eastern Samar, Philippines was featured by the Western Pacific Surveillance and Response Journal (WPSAR) describing the dangers of turtle meat consumption.1 As highlighted by the authors, 68 cases were identified with a 6% case fatality ratio (CFR). Also, the results revealed that there was a dose-dependent relationship between turtle meat or soup consumption and risk of illness.
We investigated another episode of a chelonitoxism outbreak in the village of Liang, Irosin, Sorsogon, Philippines in October 2014. A clinical chelonitoxism case was defined as a well individual who developed epigastric pain, nausea, vomiting or diarrhoea2 in the village of Liang, Irosin, Sorsogon from 8 to 10 October 2014. We reviewed medical records of all clinically defined cases at the Irosin district hospital, and we interviewed the clinically defined cases using a standard questionnaire developed by our field investigators. Questions included demographic profile and history of food intake with emphasis on the food intake time. Data were stratified by age, familial unit, food items and incubation period for analysis using Microsoft Excel.
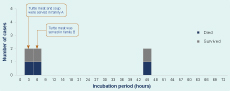
A total of six clinically defined chelonitoxism cases were identified among 33 people who ingested turtle meat (attack rate = 18%). Age of the six cases ranged from 1 to 48 years (median = 19 years). Three out of six (50%) were children aged between 1 and 5 years, four (66%) were male, and five out of six (83%) cases came from the same household. All cases had ingested turtle meat within two days of symptom onset. The most common symptoms were epigastric pain (83%), vomiting (83%) and dizziness (67%). The incubation period ranged between 1 and 45 hours (median = 4 hours). Four (66%) cases developed symptoms within 5 hours of consuming turtle meat/soup while two (33%) cases developed symptoms between 44 and 45 hours after exposure. The CFR was 50% (Figure 1). All human deaths occurred in one household. Three out of three (100%) paediatric cases (age < 5 years) died, while all three adult cases survived. Meanwhile, one household reported that two pet dogs died after eating the vomitus of one of the household members who later died.
According to the investigation results, we did not find any association between dose of turtle meat ingested and probability of survival. Two rectal swab specimens were collected from two available cases for bacteriologic culture and no enteropathogenic isolates were yielded. Unfortunately, as with many turtle meat poisoning outbreaks in south-eastern Asia,3 we were not able to confirm chelonitoxism directly via laboratory confirmation of toxins due to insufficient laboratory capacity.
Based on the results, we characterized this outbreak to be: (1) familial clustering; (2) bimodal distribution of incubation period; and (3) mortality restricted to children. As clinical case definitions for chelonitoxism are nonspecific, we recommend building referral mechanisms to existing laboratories doing chelonitoxism outbreak confirmation. Stricter enforcement of existing laws against hunting and sea turtle consumption could limit the morbidity and mortality of chelonitoxism in the Philippines and other countries with turtles as a common food source.4
None declared.
None.