a Field Epidemiology Training Program, National Epidemiology Center, Department of Health, Sta Cruz, Manila, Philippines.
b Department of Health, Sta Cruz, Manila, Philippines.
Correspondence to Ray Justin Ventura (e-mail: rayjustinventura@gmail.com).
To cite this article:
Ventura RJ et al. Chelonitoxism outbreak, Eastern Samar, Philippines, August 2013. Western Pacific Surveillance and Response Journal, 2015, 6(2):12–16. doi:10.5365/wpsar.2015.6.1.003
Background: On 21 August 2013, the Event-based Surveillance and Response system of the Department of Health, Philippines captured a foodborne illness event among residents of a coastal village in Eastern Samar, Philippines. The suspected cause was the consumption of a sea turtle found near the village. A team from the Department of Health was sent to conduct an outbreak investigation.
Methods: A case was defined as any person in Arteche, Eastern Samar, who developed dry mouth and burning sensation in the throat from 15 August to 27 August, 2013. Severity of the disease was classified as mild, moderate or severe. We conducted records review, environmental investigation, interviews of key informants and a retrospective cohort study.
Results: Sixty-eight cases were identified; four died (case fatality rate = 6%). All cases had a history of turtle meat consumption. Dose-dependent relationship was noted between amount of turtle meat consumed and the risk of illness. In the cohort study, consumption of turtle meat and turtle meat soup were associated with illness.
Conclusion: This study identified turtle meat as the source of this foodborne outbreak and emphasized the dangers of consuming turtle meat. Other reported cases of turtle meat poisoning in the Philippines suggest that turtle consumption is an ongoing practice in the country. By publishing information about sea turtle poisoning outbreaks in the Philippines, we hope to raise awareness of the potential severe health effects from ingesting these endangered sea creatures.
Chelonitoxism (sea turtle meat poisoning) is a rare and sometimes fatal type of food poisoning caused by eating marine turtles. It has been reported in subtropical Atlantic, Pacific and Indian Ocean countries.1 Green sea turtles (Chelonia mydas) and hawksbill turtle (Eretmochelys imbricata) are the species most commonly implicated. Studies show that all parts of the sea turtle are potentially toxic. Symptoms can be as mild as nausea and vomiting to more severe forms of neurologic manifestations, coma and ultimately death.2
Although legally protected in the Philippines,3 sea turtles are considered a local delicacy, especially in the coastal areas. As a result, reports of chelonitoxism have persisted in the Philippines, the earliest from 1917, when 33 cases of chelonitoxism were reported in Cebu with 14 deaths (case fatality rate [CFR] = 42%).4 In 1954, 14 cases were reported in Mindanao with 11 deaths (CFR = 79%).5 More recently in Sorsogon, six of 33 villagers (attack rate [AR] = 18%) manifested symptoms consistent with chelonitoxism after eating turtle meat.6
On 21 August 2013, the Event-based Surveillance and Response (ESR) system of the Department of Health, Philippines captured a foodborne illness event among residents of Rawis, a small village situated in the coastal area of Arteche, Eastern Samar. The suspected cause was the consumption of a sea turtle found near the village. On 27 August 2013, a team from the Department of Health was sent to conduct an outbreak investigation to verify the outbreak and identify risk factors.
A case was defined as any person in Arteche, Eastern Samar, who developed dry mouth and burning sensation in the throat from 15 to 27 August 2013. Active case finding was conducted by reviewing medical records from the Arteche Rural Health Unit and the Eastern Samar Provincial Hospital. The initial 10 cases were interviewed using a structured questionnaire with data on demographics, food and water exposures and environmental risk factors.
Severity of disease was classified as mild, moderate or severe as per standard case categorization.2 A mild case was defined as having throat pain and dryness of mouth with or without diarrhoea, dizziness, malaise and sweating. A moderate case was someone who developed any of the following: mouth ulcerations, white coated tongue or tongue fissures. A severe case was someone who developed neurological manifestations including alternating periods of lethargy and agitation or decrease in sensorium.
We conducted a retrospective cohort study among residents of Sub-village 4. A more specific questionnaire was used for the cohort study comprising questions on the amount of turtle meat consumed and consumption of turtle meat soup to obtain data on the amount of turtle meat consumed, the types of body parts consumed, consumption of turtle meat soup and participant’s sex. Analysis was done using EpiInfo version 3.5.4. We calculated relative risks (RR), 95% confidence intervals (CI), P values and food-specific AR and attack rate ratios (ARR). Risk factors approaching significance (P < 0.2) in univariate analysis were retained for multivariate logistic regression using a forward stepwise procedure.
A site visit was conducted in Sub-village 4 to identify the circumstances surrounding the event. We interviewed the Municipal Environment and Natural Resources Officer to gather data on turtle sightings, resident awareness of laws prohibiting the selling and butchering of sea turtles and to identify the implicated turtle. The fisherman who butchered and sold the implicated turtle meat was interviewed about the capture, processing and selling of the turtle meat.
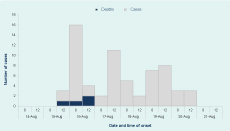
A total of 68 cases were identified. Onset of symptoms ranged from four hours to five days (median = 1.5 days) (Figure 1). Signs and symptoms included light-headedness (68%), epigastric pain (41%) and vomiting (32%). Cases appeared on the evening of 15 August 2013 and peaked in the morning of 16 August. Fifty-two people (76%) received outpatient medical care, six (9%) were hospitalized and four died (CFR = 6%).
Age of cases ranged from 2 to 80 years (median = 34 years); 74% were male. The most affected age group was 11- to 20-year-olds. All cases came from Sub-village 4. All of the cases ate turtle meat before the onset of illness. Thirty-five (51%) experienced mild symptoms, 27 (40%) were classified as moderate cases and 6 (9%) had severe manifestations.
Ages of the four deaths ranged from 23 to 80 years (median = 57 years). The onset of symptoms ranged from 24 to 46 hours (median = 34.5 hours). All fatal cases experienced severe manifestations before death. Three (75%) came from the one family. All consumed more than 10 tablespoons of turtle meat. Lethal cases also consumed turtle soup (100%), internal organs (100%), turtle eggs (75%) and the head (25%) of the turtle.
We interviewed 136 of 170 (80%) residents of Sub-village 4. Of study participants, 100 (74%) ate turtle meat. We found that being male (RR = 1.53, 95% CI: 1.03–2.27) and consuming ≥ 1/2 cup of turtle meat soup (RR = 1.62, 95% CI: 1.19–2.23) were associated with illness along with consumption of turtle meat (RR = 1.92, 95% CI: 1.28–2.88), internal organs (RR = 1.65, 95% CI: 1.19–2.30) and blood (RR = 1.60, 95% CI: 1.14–2.26). In multivariate analysis, consumption of turtle meat (RR = 4.26, 95% CI: 1.01–18.00) and consumption of ≥ 1/2 cup of turtle meat soup (RR = 6.93, 95% CI: 2.82–17.02) were the only risk factors associated with illness (Table 1).
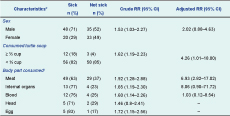
95% CI, 95% confidence interval; RR, relative risk.
* Totals may not add up due to missing responses
† May have more than one response
We found a dose–response relationship with consumption of increasing quantities of turtle meat. The AR of those who ate more than 2 tablespoons of turtle meat was 87.3% (48/55) compared to 35.2% (12/36) for those who ate 1 tablespoon of turtle meat (RR = 2.47, 95% CI: 1.5–3.94) (Table 2).
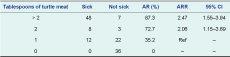
AR, attack rate; ARR, attack rate ratio; CI, confidence interval.
The village people depend on fishing as their primary source of livelihood. They knew that catching, killing and selling sea turtles is prohibited and punishable by law, but they continue to do so because of the demand for this local delicacy. Most common sea turtle species seen in the area are the green sea turtle (Chelonia mydas) and the hawksbill sea turtle (Eretmochelys imbricata).
A fisherman captured a sea turtle on 15 August 2013 at 07:00 in shallow water. He positively identified the species as Chelonia mydas. The live sea turtle was found trapped in the corals. The fisherman butchered the trapped sea turtle and sold a total of 12 kg of raw meat to the villagers within hours. No special preparation was done on the meat. The raw meat was individually prepared and cooked by several families. There was no banquet or community meal before the start of the outbreak.
After the incident, a community assembly was organized by the Municipal Health Office and the Department of Health to educate the villagers on the law prohibiting the killing of sea turtles and the dangers of consuming its meat.
This foodborne outbreak was most likely caused by consumption of turtle meat. The study revealed that 100% of cases had a history of turtle meat ingestion; none of those who did not eat turtle meat presented with symptoms. The signs and symptoms of the cases and incubation period were similar to those of other chelonitoxism outbreaks.2 The dose–response relationship provides strong evidence as to the source of the outbreak. Other studies have also demonstrated a dose–response relationship with turtle meat or turtle soup poisoning.2,7
Investigators from the Federated States of Micronesia recently reported a similar outbreak with 191 cases of chelonitoxism after consuming sea turtle stew,7 showing that the consumption of turtles is also common elsewhere. They reported a low CFR of 6%, possibly due to aggressive case ascertainment efforts. This is consistent with our CFR, although some studies have reported it as high as 100%.2
One of the limitations of this study was incomplete capture of the study population. As uncaptured residents may have been less likely to have the disease, we may have overestimated the occurrence of disease. Also, laboratory testing of specimens collected from human and animal samples was not done due to the lack of availability of testing centres. However, in this region, most sea turtle poisoning outbreaks are not usually laboratory confirmed.4–7
In conclusion, this study was able to identify the turtle meat as the source of this foodborne outbreak, emphasizing the dangers of consuming turtle meat. The persistence of chelonitoxism outbreaks in the Philippines proves that consumption of this animal is an ongoing practice in the country6 despite it being illegal. Strict implementation of the law could prevent future incidents, but the feasibility of such implementation is unclear as it is difficult to keep coastal people from consuming a traditional food source. By publishing information about sea turtle poisoning outbreaks in the Philippines, we hope to raise awareness of the potential severe health effects from ingesting these endangered animals.
None declared.
This foodborne outbreak investigation was funded by the Department of Health, Philippines.
We are grateful for the cooperation and support of the Centre for Health and Development-Eastern Visayas, Eastern Samar Provincial Health Office, Eastern Samar Provincial Hospital, Local Government Unit of Arteche and town residents during the field investigation.