a Health Protection Unit, New South Wales, North Sydney, Australia.
Correspondence to Robin Gilmour (e-mail: rgilm@doh.health.nsw.gov.au).
To cite this article:
Rosewell A et al. New South Wales annual vaccine-preventable disease report, 2013. Western Pacific Surveillance and Response Journal, 2015, 6(2):37–44. doi:10.5365/wpsar.2014.5.4.009
Aim: To describe the epidemiology of selected vaccine-preventable diseases in New South Wales, Australia for 2013.
Methods: Data from the New South Wales Notifiable Conditions Information Management System were analysed by local health district of residence, age, Aboriginality, vaccination status and organism. Risk factor and vaccination status data were collected by public health units.
Results: Pertussis notification rates in infants were low, and no infant pertussis deaths were reported. Despite a high number of imported measles cases, there was limited secondary transmission. The invasive meningococcal disease notification rate declined, and disease due to serogroup C remained low and stable.
Conclusion: Vaccine-preventable diseases were relatively well controlled in New South Wales in 2013, with declining or stable notification rates in most diseases compared with the previous year.
Monitoring vaccine-preventable diseases is important to identify events that may require immediate public health control measures and to better inform policy and targeted immunization efforts.
New South Wales is Australia’s largest state and is divided into 15 local health districts (LHDs).1 Each LHD has a public health unit responsible for follow-up of all health-related issues including vaccine-preventable diseases. Under the state’s public health legislation, medical practitioners, hospital general managers and laboratories are required to notify certain vaccine-preventable diseases.2 Upon receipt of a notification, a surveillance officer from the relevant public health unit determines whether or not the notification meets the case definition of a vaccine-preventable disease according to national criteria.3 If so, data on each notified case are entered into the New South Wales Notifiable Conditions Information Management System (NCIMS).
This report describes notification data for measles, pertussis, rubella, Haemophilus influenzae serotype b invasive infection, invasive meningococcal disease, mumps, tetanus, invasive pneumococcal disease and selected travel-related diseases in New South Wales, Australia in 2013.
Data describing cases in NCIMS were extracted for selected vaccine-preventable diseases with a date of onset in 2013. Rates were calculated using 2011 Australian Bureau of Statistics population estimates and are presented as annual rates per 100 000 total population or population in age groups. The notification rates were analysed by geographic area of residence. Risk factor and vaccination status data were collected through follow-up with either general practitioners or the Australian Childhood Immunization Register (ACIR) and other sources such as cases or health-care provider reports.
In 2013, nine cases of H. influenzae serotype b infection were notified; five were children under 5 years and six were female. All three infants under 1 year (one 1-month-old and two 9-month-old infants) were fully vaccinated for age (one and three doses respectively). Of the two infants aged 12 months or older, one 19-month-old infant was partially vaccinated for age (one dose) and one 3-year-old was fully vaccinated for age (four doses). One case was identified as being Aboriginal and five lived in regional New South Wales.
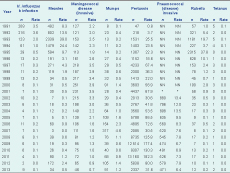
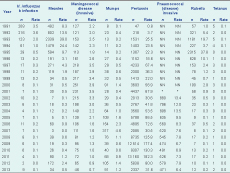
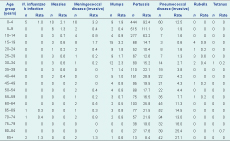
In 2013, 34 cases of measles were notified in New South Wales, compared to 172 in 2012 (Table 1). The highest notification rates were reported among children aged 0–4 years (10 cases, 2.1 per 100 000 population), of whom four were too young to be vaccinated, and in children aged 5–9 years (six cases, 1.3 per 100 000 population) (Table 2). Seventeen cases (50%) were male. Of the 34 cases of measles, 22 were Australian-born, nine were born in countries other than Australia (mostly in the Asia-Pacific region and Europe) and no data was available on three cases.
NN, not notifiable; * incomplete data. 1991–1992 data should be interpreted with caution as the notification system was just commencing.
Note: Major changes to the New South Wales Immunization Programme since 1991 include: Haemophilus influenzae serotype b immunization commencement in July 1993, second dose of measles-containing vaccine (measles–mumps–rubella, MMR) for all 10–16-year-olds recommended in 1993, Australian Measles Control Campaign: re–scheduling of the second dose of MMR to 4 years of age, catch–up vaccination for primary schoolchildren aged 5–12 years in 1998, MMR vaccine at 18 months as a replacement of MMR at four years in July 2013, conjugate meningococcal C vaccine introduction in 2003, 4CMenB registration in August 2013, the addition of a preschool pertussis booster in 1994, acellular vaccines (DTPa) replacement of the whole cell vaccine in the late 1990s, the replacement of the 18-month booster with an adolescent booster in 2003, dTpa funded by NSW for parents, grandparents and carers of infants aged < 12 months under cocoon strategy, 7-valent conjugate pneumococcal vaccination (PCV-7) for infants since 2005 and 13-valent conjugate pneumococcal vaccine (PCV-13) replaced PCV-7 from July 2011 (see link to further information – http://ncirs.edu.au/immunisation/history/index.php).
Measles cases were notified from eight LHDs; the highest rate was in the Northern New South Wales LHD (six cases, 2.1 per 100 000 population) (Table 3).

* Note: Missing and overseas-acquired notifications are not included.
N/A, not applicable.
Of the 34 cases, 18 (53%) were unvaccinated, 11 (32%) were vaccinated and five (15%) had missing vaccination status. Vaccination status was validated on the ACIR for four (all children under 5 years) and by self or parent recall for seven. Of the four cases with vaccination validated on ACIR, only one 2-year-old with mild disease had evidence of receiving two doses of vaccine.
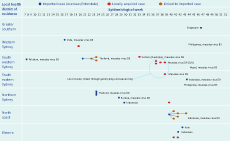
Of the 34 cases notified in 2013, 14 (41%) were acquired overseas, 19 (56%) were acquired in New South Wales, and one (3%) was acquired elsewhere in Australia. There were four cases infected with measles virus genotype B3 (acquired in the Philippines, Nepal, Pakistan), six with measles virus genotype D8 (acquired in Europe, Thailand, India, Victoria [Australia]) and six with measles virus genotype D9 (acquired in Indonesia). The longest duration of linked transmission (onset in primary case to onset in last case) was 29 days, which occurred in the largest cluster (n = 6 cases) (Figure 1).
In 2013, 46 cases of invasive meningococcal disease were notified in New South Wales compared with 65 cases notified in 2012 (Table 1). Two deaths were notified among cases in 2013; one was in the 50–54-year-old age group (serogroup C), and the other was 85 years or older (serogroup Y). This compares to two deaths in 2012 (both caused by serogroup B).
The highest case notification rates of invasive meningococcal disease were among children aged less than 5 years at onset of illness (16 cases, 3.3 per 100 000 population) and young people aged 15–19 years (eight cases, 1.7 per 100 000 population) (Table 2). Of the case notifications among children under 5 years, the highest rates were reported in infants under 12 months (six cases, 7.8 per 100 000 population) and children aged 2 years (four cases, 5.6 per 100 000 population).
In 2013, 24 cases (52%) with invasive meningococcal disease were male. Invasive meningococcal disease was notified in four Aboriginal people, all due to serogroup B infection. The highest case notification rates were from Northern New South Wales LHD (four cases, 1.4 per 100 000 population) (Table 3).
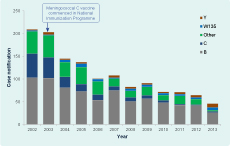
Of the 46 cases notified in New South Wales in 2013, a serogroup was identified for 43 (93%): 26 (60%) cases were serogroup B (for which there was no vaccine), eight (19%) were serogroup Y, six (14%) were serogroup W135, and three (7%) were serogroup C. Of the three untyped cases, two were not typeable (Figure 2). Of the three cases of disease due to serogroup C, two were ineligible for vaccination through the National Immunization Programme, and one was vaccinated against meningococcal C disease in 2004. The overall decline in notifications from 2012 to 2013 was associated with a decline in serogroup B disease from 43 to 26 notifications (Figure 2).
In 2013, 91 cases of mumps were notified in New South Wales compared to 105 in 2012 (Table 1). The highest case notification rates of mumps were among young adults aged 15–19 years (15 cases, 3.2 per 100 000 population) (Table 2). In 2013, 50 cases (55%) were male. In New South Wales, notified cases of mumps are not routinely followed up by public health units.
In 2013, 2337 cases of pertussis were notified in New South Wales compared to 5838 in 2012 (Table 1). The highest age-specific pertussis case notification rates were in children aged 5–9 years (515 cases, 111.1 per 100 000 population) and 0–4 years (444 cases, 92.4 per 100 000 population) (Table 2), a decrease from 2012. Of the children under 5 years, the highest notification rates were in children aged 3 years (115 cases, 157.1 per 100 000 population). Notification rates among infants under 12 months decreased from 2012 to 2013. There were no infant pertussis deaths in 2013.
In 2013, 1324 cases (57%) were female. Of the 444 cases aged 0–4 years, 37 (8%) were Aboriginal. Geographically, the highest case notification rates were reported in Murrumbidgee (including Albury) (245 cases; 84.8 per 100 000 population) and Southern New South Wales (129 cases; 64.4 per 100 000 population) (Table 3).
In total, 102 cases were younger than 12 months: 56 (55%) were infants too young to have received three doses of vaccine. Of the 342 cases aged 1–4 years, 24 (7%) were reported to be not immunized, nine (3%) reported less than three doses of vaccine and 289 (85%) reported three or more doses. For the remainder of cases (5%), vaccine dosages were not reported.
In 2013, 471 cases of invasive pneumococcal disease were notified compared to 579 in 2012 (Table 1). Forty deaths occured: two were children, one aged 1-year-old (serotype 15C, non-vaccine type) and one 2-year-old (19A, vaccine type, child fully vaccinated). Of the remaining deaths, two were people aged 35–49 years, eight were 50–64-year-olds and 28 were aged 65 years and older. Notification rates by LHD varied from 3.2 per 100 000 population in Far West LHD to 9.0 per 100 000 population in Nepean Blue Mountains LHD (Table 3). Of the 361 cases aged 0–4 years or older than 50 years (age groups which are followed up by public health units), 10 (3%) were notified in Aboriginal people, among whom notification rates were higher than in non-Aboriginal people (17.0 and 11.9 per 100 000, respectively).
Notification rates in children under 5 years was 12.5 per 100 000 population. Serotype 19A was the leading cause of disease (22%) in children under 5 years. Vaccination data were available for 100% (60 cases) of notifications under the age of 5 years. Forty (67%) cases were fully vaccinated, and eight (13%) were either partially vaccinated or too young to have received the first dose. There were eight cases of vaccine serotype disease in fully vaccinated children. Serotype 19A accounted for 63% of vaccine failures and serotypes 3 (25%) and 23F (12%) were responsible for the remainder of cases. From 1 July 2011, 13-valent conjugate pneumococcal vaccine (PCV-13) replaced 7-valent conjugate pneumococcal vaccine (PCV-7) on the New South Wales immunization schedule. The PCV-13 vaccine includes protection for additional serotypes 1, 3, 5, 6A, 7F and 19A. The rate of disease in children under 5 years in New South Wales declined from 19.0 per 100 000 in 2011 to 12.5 per 100 000 in 2013 after the introduction of PCV-13. The percentage of disease due to vaccine serotypes fell by 29% post introduction; however, the percentage of disease due to non-vaccine serotypes increased by 29%.
In 2013, 12 cases of rubella were notified in New South Wales compared to 10 in 2012 (Table 1). All cases were aged between 15 and 60 years. Seven cases (58%) were male. The highest notification rates were in the Northern New South Wales LHD (six cases, 2.0 per 100 000 population) (Table 3). Notifications have not changed markedly over the previous five years.
In 2013, two cases of tetanus were notified in New South Wales. One case was a 30-year-old male construction worker who reported being vaccinated. The other was an 82-year-old male who reported being vaccinated more than 10 years earlier.
The number of notified cases of tetanus has remained relatively unchanged over the past five years, ranging from one to two cases annually.
In 2013, two cases of cholera were notified in New South Wales. One case in an unvaccinated person was acquired during a visit to Bangladesh, and an occupationally acquired case was notified in a laboratory worker.
In 2013, 62 cases of hepatitis A were reported of which 47 (75%) were acquired overseas. One case reported vaccination against hepatitis A five years before leaving Australia. Another seven (11%) were household contacts of those that had travelled overseas, and two (3%) reported consuming food acquired overseas. The remaining six (10%) cases were acquired locally with no source identified.
In 2013, there were 59 notifications of typhoid; 54 (93%) were acquired overseas. Of these 54 notifications, six reported being vaccinated against typhoid before travelling. Five cases reported no overseas travel. Of these, three had household contact with a confirmed case, one reported contact with overseas visitors, and the source was not identified for one case.
In 2013, pertussis notification rates were the lowest across all age groups since 2007. The 2013 pertussis epidemiology is consistent with a low transmission period in the three- to four-year cycle of pertussis epidemics. The high vaccination coverage among adult caregivers during the New South Wales Health funded cocooning vaccination programme may have also contributed to the low rates.4 As with previous years, the highest notification rates were in 5–9-year-old children.
Endemic measles has been eliminated in New South Wales since the late 1990s;5 however, outbreaks of increasing size and duration were reported in New South Wales in 2011 and 2012.6,7 In 2013, measles epidemiology was characterized by a high number of overseas-acquired infections (n = 14, 41%) with little secondary transmission. This was likely due to high levels of immunity to measles among contacts of cases and effective systems for public health response. The highest notification rates were reported in Northern New South Wales LHD where vaccination coverage rates are the lowest in New South Wales.7
The number of notified cases of invasive meningococcal disease has declined significantly since the National Meningococcal C Immunization Programme commenced in 2003.8 Serogroup B remains predominant in New South Wales; however, the largest serogroup-specific reduction in meningococcal notifications in 2013 compared to 2012 was for serogroup B notifications in the absence of vaccination.9 The death in an elderly person due to serogroup Y is a reminder of increased mortality in the elderly, particularly for this serogroup.10 The meningococcal C vaccine failure may have been due to waning immunity, host factors or issues with the storage or administration of the vaccine. With the newly available vaccine against meningococcal serogroup B disease (not included in the current immunization schedule), consideration should be given to the potential impact on strain variation and carriage, adverse events following immunization, as well as how vaccine effectiveness and failure will be defined and monitored following its introduction.11
The H. influenzae serotype b immunization programme, which commenced in 1993, has achieved great success in achieving and maintaining low notifications for several years; notifications of other vaccine-preventable diseases (such as mumps, rubella and tetanus) have remained stable or declined over recent years. While there are limitations to these data, vaccine-preventable disease surveillance in New South Wales enables the implementation of timely public health measures, a better understanding of disease trends and informs policy.
The extremely low number of cholera, hepatitis A and typhoid cases that were vaccinated before travelling to high-risk countries highlights the great potential for pre-travel immunization. Health-care providers who see travellers before travel should consider country- and region-specific vaccination, prophylaxis, and disease avoidance recommendations during the consultation.12 Employers should implement a comprehensive occupational vaccination programme for workers at significant risk of acquiring a vaccine-preventable disease.13 The Australian Immunization Handbook could consider the inclusion of cholera (and possibly other pathogens) under recommendations for vaccination of those routinely working with this pathogen.
Invasive pneumococcal disease continued to decline post introduction of the 13-valent conjugate pneumococcal vaccine in 2011 with overall reduction of disease in the majority of age groups. Notification rates in children under 5 years in New South Wales has fallen from 19.0 per 100 000 in 2011 to 12.5 per 100 000 in 2013. Serotype 19A continues to be the leading cause of disease in children and also accounts for the majority of vaccine failures in this age group (0–5 years). While notification rates are not increasing in children, notification rates caused by non-vaccine-related serotypes continue to increase.
Notifications included in the New South Wales notifiable disease database under the Public Health Act 201014 have laboratory evidence or a link to a laboratory-confirmed case. The number of notifications reflects health-care-seeking behaviour and testing practices which vary across New South Wales. Consequently, the data analysed likely understates the true incidence of infection in New South Wales.
Vaccine-preventable disease surveillance has enabled enhanced monitoring of disease trends, implementation of outbreak control measures and evaluation of prevention programmes in New South Wales. The highlights of the prevention and control programmes in 2013 include the low pertussis notification rates in infants, no infant pertussis deaths, extremely limited measles transmission following overseas importation and low rates of invasive meningococcal disease due to serogroup C. Challenges remain in closing the measles immunity gaps in at-risk populations, ensuring new mothers have been adequately immunized against pertussis (and influenza) as well as improved uptake of vaccination in travellers and other risk groups. High vaccination coverage and timely vaccination for infants and children is important to maintain low rates of disease. Improving vaccination coverage in Aboriginal communities is crucial for successful disease prevention strategies.
None declared.
None.
We wish to acknowledge disease notifiers and Public Health Network staff who conduct investigations and follow up notifications and the New South Wales Health Laboratory Network.