a Health Protection Unit, New South Wales, Australia.
Correspondence to Alexander Rosewell (e-mail: arosw@doh.health.nsw.gov.au).
To cite this article:
Rosewell A et al. New South Wales annual vaccine-preventable disease report, 2012. Western Pacific Surveillance and Response Journal, 2014, 5(2). doi:10.5365/wpsar.2014.5.2.004
We aim to describe the epidemiology of selected vaccine-preventable diseases in New South Wales (NSW) for 2012. Data from the NSW Notifiable Conditions Information Management System were analysed by: local health district of residence, age, Aboriginality, vaccination status and organism, where available. Risk factor and vaccination status data were collected by public health units for cases following notification under the NSW Public Health Act 2010. The largest outbreak of measles since 1998 was reported in 2012. Pacific Islander and Aboriginal people were at higher risk as were infants less than 12 months of age. Notifications of invasive pneumococcal disease (IPD) in children less than five years declined; however, the overall number of notifications for IPD increased. Mumps case notifications were also elevated. There were no Haemophilus influenzae type b case notifications in children less than five years of age for the first time since the vaccine was introduced. Invasive meningococcal disease case notifications were at their lowest rates since case notification began in 1991. Case notification rates for other selected vaccine-preventable diseases remained stable. Vaccine-preventable disease control is continually strengthening in NSW with notable successes in invasive bacterial infections. However, strengthening measles immunization in Pacific Islander and Aboriginal communities remains essential to maintain measles elimination.
New South Wales (NSW) is the most populous state in Australia with a resident population of approximately 7.3 million. The objectives of vaccine-preventable disease surveillance in NSW are, at an individual level, to identify events that may require immediate public health control measures and, at a population level, to identify risk factors such as age and geographic location that inform better targeted immunization efforts. This report describes case notification data for measles, pertussis, rubella, Haemophilus influenzae type b invasive infection, invasive meningococcal disease (IMD), mumps, tetanus and invasive pneumococcal disease (IPD) in NSW, Australia, in 2012 and provides comparison with recent trends.
The case notification requirements for medical practitioners, hospital general managers and laboratories under the state’s public health legislation have been previously described.1 On receipt of a case notification, a public health unit surveillance officer determines whether or not the case notification meets the definition of a case of vaccine-preventable disease according to national criteria2 and if so enters data gathered on each case into the NSW Notifiable Conditions Information Management System (NCIMS). Data describing cases in NCIMS were extracted for selected vaccine-preventable diseases according to the date of onset, with 2012 data compared with data for recent years. Rates were calculated using Australian Bureau of Statistics population estimates and are presented as annual rates per 100 000 total population or population in age groups.3 Risk factor and vaccination status data were collected for cases through public health unit follow-up with general practitioners and other sources such as case or caregiver reports. The incidence of cases were analysed by geographic area of residence. All analyses were performed using SAS Enterprise Guide 6.1 (SAS Institute Inc., Cary, NC, USA) and Microsoft Excel 2010 software (Microsoft Corporation, USA).
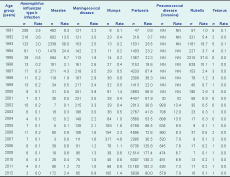
In 2012, two cases of Haemophilus influenzae type b infection were notified; this was the lowest number of cases notified within the last decade and the first time since the introduction of the vaccine in 1993 that no cases were notified in children less than five years of age (Table 1).
NN, not notifiable; ID, incomplete data.
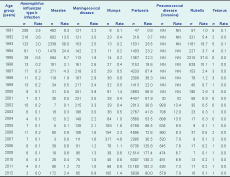
There were 172 cases of measles notified in NSW in 2012 compared to 90 in 2011. Of the outbreak associated cases, 12 (7.1%; 5.8 per 100 000 population) were identified as Aboriginal people (Figure 1) with Pacific Islander people disproportionately affected, particularly people of Samoan ancestry (17.3%; 188.7 per 100 000 population). Age group and local health district-specific measles notification rates varied considerably (Tables 2 and 3). Many (21.4%) notifications acquired their illness in health facilities. Of the 172 cases, 102 (59.3%) were unvaccinated, 41 (23.8%) were vaccinated and 29 (16.9%) had missing vaccination status. Of the 41 cases reported as vaccinated, two had two documented doses of measles-containing vaccine, 15 had one documented dose only and the remainder did not have documented evidence on the number of doses of vaccine that they had received. Of the 172 cases, two (1.2%) were acquired overseas, 169 (98.3%) were epidemiologically or virologically linked to a Thailand-acquired case (measles virus genotype D8) and one case (0.6%) had no link to an overseas-acquired case.


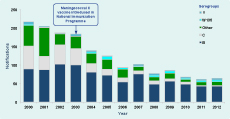
In 2012, 65 cases of IMD were notified in NSW (64 confirmed and one probable [clinical evidence only]) compared with 72 cases notified in 2011; 65 is the lowest number of cases since 1991. Three deaths among cases were notified in 2012 across a wide age range, including one seven-month-old infant, one 47-year-old and one 85-year-old (all caused by serogroup B). This compares to four deaths in 2011 (all caused by serogroup B).
Of the 65 cases notified in NSW in 2012, a serogroup was recorded for 54 (83.1%) (Figure 2). Of these 54 cases, 43 (79.6%) had disease caused by serogroup B infection (for which there was no vaccine), 42.9% of these cases were aged less than five years, 14.3% were aged 15–19 years and 14.3% were aged 45–49 years. For five cases (9.3%), disease was caused by serogroup Y infection; two of these five cases (40%) were aged 85 years or older with others aged between 20 and 49 years of age. For four cases (7.4%), disease was caused by serogroup W135 infection (of these people one was aged one year, two were aged 60–64 years and one at least 85 years of age). Only two cases (3.7%) had disease caused by serogroup C infection, and both were ineligible for vaccination under the National Immunization Programme and were not vaccinated.
There were 105 cases of mumps notified in NSW in 2012, compared to 68 in 2011. The highest mumps case notification rate was among young adults aged 30–34 years (27 cases, 5.3 per 100 000 population). In NSW, notified cases of mumps are not routinely followed up by public health units.
In 2012, 5838 cases of pertussis were notified in NSW, compared with 13 183 in 2011. One death was reported in an unvaccinated seven-week-old infant from the Illawarra Local Health District. In 2012, 2625 cases (45.0%) were male. Of the 1182 cases aged zero to four years (who are followed up by public health units), 69 (5.8%) were Aboriginal children with 12% missing/unknown.
Of the 247 cases aged less than 12 months, 157 (63.6%) were infants too young to have received three doses of vaccine (i.e. aged six months or less at onset of illness). Of the 935 cases who were children aged zero to four years, 71 (7.6%) were reported to be not immunized, 24 (2.6%) reported less than three doses of vaccine, and 798 (85.4%) reported three or more doses. Data on vaccine doses were not reported for the remaining 42 (4.5%) cases.
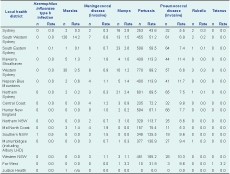
In 2012, 583 cases of IPD were notified compared to 524 in 2011 (Figure 3). Forty-four deaths were identified in 2012. There were no deaths reported in children. Of the 383 cases aged either zero to four years or older than 50 years (age groups which are followed up by public health units), 14 (3.7%) were notified in Aboriginal people among whom case notification rates were significantly higher than in non-Aboriginal people (24.8 and 13.0 per 100 000, respectively).
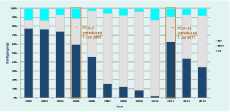
* PCV–7 includes serotypes 4,6B, 9V, 14, 18C, 19F and 23F introduced into immunization schedule.
** PCV–13 includes serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F and 23F introduced into immunization schedule.
NT, isolate not typed; NVT, non vaccine type (percentage of disease caused by serotypes not included in the vaccine); VT, vaccine type (percentage of disease caused by serotype included in the vaccine).
Vaccination data were available for 94% (61 cases) of notifications under the age of five years. Forty-four (72%) cases were fully vaccinated and 17 (28%) cases were either partially vaccinated or too young to have received their first dose. There were two vaccine failures, and both cases were fully vaccinated and both cases’ disease was caused by serotype 19F. Since 1 July 2011, 13-valent pneumococcal conjugate vaccine (PCV-13) replaced 7-valent pneumococcal conjugate vaccine (PCV-7) on the NSW immunization schedule. The PCV-13 vaccine includes protection for additional serotypes 1, 3, 5, 6A, 7F and 19A. The rate of disease in children under the age of five years in NSW after the introduction of PCV-13 declined from 19.0 per 100 000 pre-vaccine (2010) to 12.2 per 100 000 (2012). The proportion of vaccine-related disease fell by 16% post introduction; however, the proportion of non-vaccine-related disease increased by 12% (Figure 3).
In 2012, 10 cases of rubella were notified in NSW compared to 17 in 2011. Cases were aged between 12 months and 46 years. There were no case notifications of congenital rubella.
One case of tetanus was notified in NSW in 2012. This case resided in the Far West Local Health District and was an elderly female who reported never receiving a tetanus vaccination.
Prior to the commencement of immunization, Haemophilus influenzae type b was an important cause of invasive bacterial disease in children.4 Since the introduction of the vaccine, case notifications have declined substantially. In 2012, there were no case notifications in children aged less than five years for the first time in NSW. Infants should receive a Haemophilus influenzae type b containing vaccine at six to eight weeks, four and six months of age followed by a final dose at 12 months.5
Endemic measles transmission has been eliminated in Australia since 1999.6 In NSW, outbreaks occur in association with international travel but are usually of limited size and duration.7 In 2012, an outbreak associated with travel to Thailand resulted in sustained measles transmission for nine months, the largest outbreak since 1997. Similar to some measles outbreaks in 2011,8 the outbreak disproportionately affected Aboriginal and people of Pacific Islander background, particularly those of Samoan heritage.9 Higher measles notification rates in Aboriginal people may have been associated with suboptimal vaccination timeliness and coverage in selected locations; however several notifications also occurred in infants too young to be vaccinated. Improved timeliness and coverage are currently being addressed through various initiatives, including the ‘Save the Date to Vaccinate’ campaign and the recently created Aboriginal Immunization Health Worker positions based in Local Health Districts. As with other outbreaks in elimination settings, the highest case notification rates were seen in infants too young to be vaccinated (less than one year old).10 However, adolescents aged 15–19 years were also a feature of the outbreak, with high case notification rates possibly reflecting the lower immunity identified in children aged 10–14 years old in NSW in a recently published serosurvey from 2007.11 Recent measles epidemiology highlights the need for supplementary targeted vaccination efforts in teenagers and in people of Pacific Islander background and for increased measles immunity among residents travelling overseas.
Pertussis transmission is cyclical in Australia with outbreaks occurring every three to four years.5 The highest number of pertussis case notifications was reported in 2011 (a continuation of the 2010 epidemic period). Case notifications declined substantially in 2012 to the lowest number since 2008 (when a more sensitive test became widely adopted). Vaccination remains the cornerstone of pertussis prevention and control and aims to prevent severe pertussis and deaths which mostly occur in infants less than two months of age.1212 Recent evidence generated in NSW and internationally indicates that adult vaccination is most effective at preventing pertussis in babies when given to women planning a pregnancy or in the third trimester of pregnancy.13 Whooping cough vaccination is strongly recommended for adults in contact with babies too young to be vaccinated.5
In Australia, the number of IMD case notifications continues to decline since the introduction of the meningococcal C vaccine in 2003.14 The greatest reduction in notified cases of meningococcal disease has been for serogroup C, from 45 cases (29% of those with known serogroup) in 2003 to less than 10 cases annually over the past five years and two cases (4% of those with known serogroup) in 2012. Neither of the two cases of meningococcal C disease was eligible for vaccination in Australia. The number of cases of meningococcal disease associated with serogroup B has also decreased over time but remains the most commonly identified serogroup. The case notifications of other serogroups (W135 and Y) have remained low and stable in recent years. A meningococcal B vaccine has recently been added to the Register of Therapeutic Goods but is not included in the National Immunization Programme Schedule. Given that all meningococcal deaths in 2011 (n = 4) and 2012 (n = 3) were caused by serogroup B disease, there is potential for mortality reduction if parents choose to vaccinate their children.
Following the introduction of PCV-7 in 2005 for children under five years, there has been a reduction in IPD due to these seven serotypes. There was a steady increase in IPD due to other serotypes (predominantly serotypes 1, 3, 6A, 7F and 19A) before the introduction of PCV-13 vaccine in 2011. The overall reduction in IPD in children under five years is however not as significant as the reduction seen in 2005 with the introduction of PCV-7. Reductions in case notifications for other age groups are not yet evident. In fact, the overall number of IPD cases increased in 2012 compared with 2011; however, this could be as a result of the severe influenza season experienced by NSW in 2012, as influenza is a risk factor for IPD.15 Replacement disease with non-vaccine serotypes is already apparent and will need to be monitored for future impact on disease burden.
Vaccine-preventable diseases are generally well controlled in NSW; however, high vaccination coverage and timely vaccination for infants and children remain crucial to maintain low rates of disease. While the lack of Haemophilus influenzae type b case notifications among young children for the first time since vaccination was introduced reflected the success of the immunization programme, supplementary initiatives are required to improve adolescent vaccination coverage in specific ethnic populations, particularly people of Pacific Islander background in parts of metropolitan Sydney. Pertussis case notifications have declined; however, vaccination remains strongly recommended for adults in contact with babies too young to be vaccinated. The burden of travel-associated vaccine-preventable diseases highlights the need for travellers to ensure they are appropriately vaccinated before their departure.
Surveillance summaries are exempt from ethics approval with the NSW Health system.
None declared.
None.
We wish to acknowledge disease notifiers and Public Health Network staff who conduct investigation and follow-up of notifications, as well as the NSW Health Laboratory Network.