a New South Wales Public Health Officer Training Program, New South Wales Ministry of Health, Australia.
b School of Public Health and Community Medicine, University of New South Wales, Australia.
c Population Health, Hunter New England Local Health District, New South Wales, Australia.
d Communicable Diseases Branch, Health Protection, New South Wales Ministry of Health, North Sydney, Australia.
e New South Wales Refugee Health Service, Sydney, Australia.
f Hunter Medical Research Institute, Newcastle, New South Wales, Australia.
Correspondence to Emma Quinn (e-mail: equin@doh.health.nsw.gov.au).
To cite this article:
Quinn E et al. Improving ethnocultural data to inform public health responses to communicable diseases in Australia. Western Pacific Surveillance and Response Journal, 2014, 5(2). doi:10.5365/wpsar.2014.5.1.011
It is well established that ethnocultural groups of migrants are associated with a differential risk of communicable disease, including measles, tuberculosis and hepatitis B. Global public health agencies1 are now focusing on improving the collection of ethnocultural data to better define communicable disease risk in migrant populations to support community-level disease prevention and control.
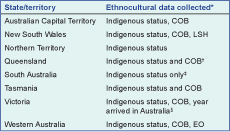
In Australia, there is no national strategy to support the collection of ethnocultural data in communicable disease surveillance. Ethnocultural data refers to any data that identifies an individual’s cultural heritage, background or affiliation, e.g. country of birth (COB); language spoken at home (LSH) or religious affiliation etc. In Australia, Aboriginal and Torres Strait Islander status is routinely collected in communicable disease surveillance. COB is commonly collected for most notifiable diseases, however other variables used to describe the ethnocultural identity of cases vary (Box 1). These data are collected either via general practitioners recording this information on the disease notification form and/or public health unit staff recording the data during follow-up interviews with individual cases.
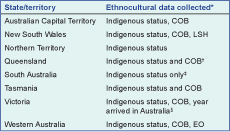
COB – country of birth, LSH – language spoken at home, EO – ethnic origin/ethnicity (Indigenous status or other). Indigenous status includes options of Aboriginal only, Aboriginal and Torres Strait Islander, Torres Strait Islander only or neither Aboriginal or Torres Strait Islander for identification purposes.
* As listed on the state or jurisdiction-specific notifiable diseases form online and/or through personal communication with state and territory Health Departments.
† Data on ethnicity and whether English is the preferred language spoken at home (Y/N) are collected in Queensland for some notifiable diseases.
‡ COB and LSH not routinely collected in South Australia but included for some priority notifiable diseases, i.e. sexually transmitted infections and food-related diseases.
§ Only collected for individuals born overseas.
Ethnocultural identity is a self-constructed phenomenon related to the many social and cultural factors that influence people’s lives including migration status, religious affiliation, language, cultural practices and political ideologies.2 Collecting valid ethnocultural data can be challenging because ethnocultural identity is not a singular and easily defined concept. Ethnocultural identity may change over time and it often changes unpredictably over subsequent generations.2 Therefore, Australian standards3 for the collection of such data reflect the need for a multidimensional concept of ethnocultural identity, including several variables to ensure reasonable specificity and sensitivity.
Despite these challenges, the ethnocultural data currently collected during routine communicable disease surveillance have assisted in disease prevention and control in Australia. Collecting COB data, though limited in scope, has helped to identify a differential disease burden in recently arrived migrants or refugees, leading to national targeted prevention and treatment programmes for migrants emigrating from countries with high-burden disease, e.g. tuberculosis and chronic hepatitis B in South Asian migrants.4
While COB helps to identify disease risk in newly arrived refugees or migrants, communicable disease risk related to ethnocultural group remains underexplored for generations of Australian-born residents. This is an important issue in a context where net overseas immigration increased two to threefold in the past decade, and second and third generation Australians now make up 20% and 53% of the population, respectively.5
The ad hoc collection of ancestry data as determined by the Australian Bureau of Statistics (ABS) in a recent outbreak investigation in New South Wales has illustrated its utility over COB and LSH for defining at-risk populations. During the 2012 measles outbreak in New South Wales, ancestry data revealed that 21% of all notifications were associated with Australians of Pacific Islander ethnicity, and 17% occurred in Pacific Islanders with Samoan ethnicity.6 This understanding enabled a quantification of the measles risk for this ethnocultural group at more than 50 times the non-Samoan population (notification rates of 189 per 100 000).6 This led to targeted public health action, including vaccination clinics in churches and schools attended by a large number of young-adult Pacific Islanders, particularly for those of Samoan descent. Culturally specific and language-appropriate communication materials were also developed.
Foodborne disease outbreaks caused by the consumption of culture-specific foods are also common in New South Wales.7 The utility of collecting data on the ethnocultural background of cases has been highlighted in New South Wales as it prompts the inclusion of ethnic food-specific questions into routine investigation tools. These specific food-related risks are inadequately identified by COB or LSH alone. To further explore which additional data variables might be useful to accurately represent ethnocultural identity, we used previously established surveillance criteria8 to review commonly used variables. As shown in Table 1, COB and LSH have conceptual validity, objectivity and are relatively easy to define. However, the inherent strengths of variables such as ethnicity or ancestry include self-determination of cultural identity and the ability to describe the ethnocultural background of non-Aboriginal and Torres Strait Islander Australian-born residents.

ABS – Australian Bureau of Statistics; DIBP – Department for Immigration and Border Protection.
* The criteria include8 conceptual validity, measurement validity, exclusivity/exhaustiveness, meaningfulness, reliability, consistency and flexibility.
A national approach to ethnocultural data collection may enable the strengthening of disease control for at-risk populations. We recommend that surveillance of COB and LSH be maintained in New South Wales and considered in other relevant jurisdictions. However, the collection of data on ancestry or ethnicity for defining communicable disease risk in multicultural groups (above and beyond COB and LSH) is warranted in Australia, particularly as social and cultural practices influence disease risk, in combination with a variety of other factors.9
The collection of data according to the ABS Australian Standard Classification of Cultural and Ethnic Groups10 in our routine communicable diseases surveillance would be valuable for estimating disease risk in generations of Australians that identify with particular cultural and/or ancestral groups. Denominator data would be available online from the ABS website via the population census carried out every five years. Estimation of disease risk related to ancestry would be helpful during outbreaks of notifiable diseases where transmission risk is associated with social or cultural practices, e.g. consumption of culturally-specific foods, cultural gatherings or family-related travel to disease-endemic countries. This type of information would help inform specific community-level prevention and control activity.
Further discussion is needed regarding acceptability, database development needs, resource implications and training required to introduce new variables into the routine surveillance of communicable diseases in Australia. The development of strategies to collect these data could follow existing best practice guidelines on how to implement, collect and use data appropriately on Aboriginal and Torres Strait Islander peoples. Consideration of enhanced surveillance of ethnocultural background could initially be given for a small number of specific diseases such as measles and meningococcal disease, which cause significant morbidity and/or mortality, where notifications are routinely followed up by public health staff and where socio-cultural practices may play a role in transmission.
None declared.
None.
The first author was employed as part of the New South Wales Public Health Officer Training Programme, funded by the New South Wales Ministry of Health. The study was conducted while the trainee was on placement in the Public Health Unit in Tamworth, Hunter New England Population Health.