a National Center for Laboratory and Epidemiology (NCLE), Ministry of Health, the Lao People’s Democratic Republic.
b Emerging Disease Surveillance and Response Unit, World Health Organization, the Lao People’s Democratic Republic.
c Oxford University Clinical Research Unit, National Hospital for Tropical Diseases, Hanoi, Viet Nam.
d Nuffield Department of Medicine, Oxford University.
Correspondence to Hannah C Lewis (e-mail: h.lewiswinter@yahoo.co.uk).
To cite this article:
Khampapongpane B et al. National dengue surveillance in the Lao People’s Democratic Republic, 2006–2012: epidemiological and laboratory findings. Western Pacific Surveillance and Response Journal, 2014, 5(1):7–13. doi:10.5365/wpsar.2014.5.1.001
Although dengue has been a public health problem for several decades in the Lao People’s Democratic Republic, the magnitude of the disease burden and epidemiological trends remain poorly understood. We analysed national dengue surveillance and laboratory data from 2006 to 2012 by person, place and time. Between 2006 and 2012, the annual dengue notification rate ranged between 62 and 367 cases per 100 000 population with an apparent geographical expansion of transmission throughout the country in recent years and concurrent co-circulation of all four dengue virus subtypes. An electronic database, called Lao Early Warning Alert and Response Network, was introduced in 2008 to provide automated early warning for outbreaks and epidemics. Village outbreaks continue to be notified primarily through event-based surveillance, whereas the weekly indicator-based system provides systematic assessment of annual epidemic cycles. The dengue case data indicate a high and increasing burden of disease. Efforts now need to focus on using available data to prompt more effective outbreak response and to guide the design and implementation of intervention strategies.
Dengue is the most rapidly spreading mosquito-borne viral disease in the world; the disease is caused by infection with one of four related viral serotypes (DEN1–4), vectored primarily by Aedes aegypti mosquitoes. It was recently estimated that there are 390 million dengue infections per year worldwide, with more than two thirds of the burden being borne by Asia.1
The Lao People’s Democratic Republic is one of the least developed countries of South-East Asia, with an estimated population of only 6.5 million in 2012 living in predominantly rural agricultural communities. The country is landlocked, but there are increasing trade and traffic linkages with other dengue-endemic neighbouring countries. In 2013, the country experienced the worst dengue fever epidemic on record; consistent with global dengue emergence, the local patterns of transmission appear linked to increasing urbanization.2 Although dengue has been a public health problem for several decades in the Lao People’s Democratic Republic, with high levels of endemicity, in urban and peri-urban areas, the magnitude of the disease burden and epidemiological trends remain poorly understood. In this report we summarize national dengue surveillance and laboratory data over a seven-year period (2006–2012).
Dengue surveillance in the Lao People’s Democratic Republic is included within the indicator-based National Surveillance System for Notifiable Selected Diseases that consists of passive weekly reports of clinically suspected cases, on admission, from all health-care facilities across the country. The case data comprise gender, age, date of onset, geographic locators (village, district, province) and case severity classifications. Between 1998 and 2010, dengue case definitions were based on the 1997 WHO guidelines3 for dengue fever, dengue haemorrhagic fever and dengue shock syndrome. From 2011, revised WHO case classifications4 were adopted: dengue without warning signs, dengue with warning signs or severe dengue (SD). Data reporting was paper-based until 2008 when an electronic database with automated early warning alerts was introduced called Lao Early Warning Alert and Response Network (Lao EWARN). Data inputted into Lao EWARN consist of weekly case numbers and deaths stratified by case classification and aggregated by province and district. Outbreak alerts are signalled when the number of dengue cases exceeds the historical mean or whenever one or more suspected cases of SD are reported. Epidemic alerts are signalled when case numbers exceed two standard deviations above the historical mean. Historical means are usually based on five years of reported data (epidemic years are excluded). Epidemic years are defined as those with reported dengue cases markedly over epidemic thresholds throughout the dengue season and/or when the health care system is overwhelmed (i.e. a shortage of hospital beds).
The National Center for Laboratory and Epidemiology (NCLE) has maintained a database of outbreaks since 2007 that includes outbreaks identified by health workers and community members (event-based surveillance) and outbreaks identified through the Lao EWARN system. When suspected dengue outbreaks are notified, response teams may be sent to collect sera from a target of 10 acute cases (fever onset less than seven days). Onsite field testing of sera using rapid diagnostic tests (RDTs) is performed if kits are available. Specimens are transferred to NCLE on wet ice by bus or air for further laboratory diagnostics. Between 2006 and 2012, laboratory diagnosis of dengue at NCLE was conducted by dengue IgM and IgG RDTs (various suppliers), commercial dengue IgM and IgG capture enzyme-linked immunosorbent assay (ELISA) (Panbio, Australia), haemagglutination inhibition assays (for epidemiological serosurveys only)5 and real-time polymerase chain reaction (RT–PCR). RDT kits including NS1 antigen (Dengue Duo NS1 Antigen + IgM/IgG, Standard Diagnostics Inc., Republic of Korea) were introduced from late 2009 and dispatched to the field. Molecular serotyping by RT–PCR was first introduced in 2006, using a conventional two-step assay performed on acute sera,6 and a real-time RT–PCR protocol was adopted in 2012.7 Starting in 2007, a testing algorithm was adopted whereby all sera submitted for analysis were tested by IgM capture ELISA, and a subset representing geographically diverse outbreaks were screened by RT–PCR. Cases were considered laboratory confirmed if the sera were processed at NCLE and tested positive for dengue IgM antibodies by ELISA or for dengue virus via RT–PCR. Convalescent sera were only rarely collected and tested.
Case data presented here comprise data extracted from the Lao EWARN database available from 2006 and validated in 2013. Case fatality rates (CFRs) were estimated based on the ratio of deaths to total reported cases. Age and gender of suspected cases were only actively collected from provinces by NCLE during the dengue epidemic in 2010. Laboratory data were extracted from log books going back to 2000. The results from the RDTs containing NS1 antigen were not available for analysis. Descriptive analyses were conducted using Excel, Epi Data Analysis v2.2 and ArcView. The chi-square test was used for bivariate analyses.
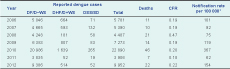
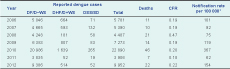
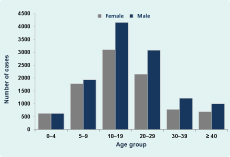
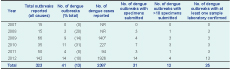
Between 2006 and 2012, the annual dengue notification rate ranged between 62 to 367 cases per 100 000 population (Table 1). The CFR was 0.2% for all years except for 2008 when it was significantly higher at 0.5% (P < 0.01). In the epidemic year of 2010, 22 890 cases and 46 deaths were reported (estimated 367 cases per 100 000 population). The largest number of cases occurred among 10-to 20-year-olds (34%) with significantly more males (12 000 cases) than females (9119 cases, P < 0.01); male–female ratio: 1.3:1 (Figure 1). Case reporting by province for 2008 to 2012 indicated a marked expansion of geographic range (Figure 2). The number of provinces with a notification rate ≥ 200 per 100 000 increased from one in 2006–2008 to five in 2009 and to 10 in 2010 (the first year that all provinces in the country reported dengue cases). Two provinces had notification rates of ≥ 200 per 100 000 in 2011, and in 2012 this increased to six provinces. Outbreaks were reported almost exclusively from urban and peri-urban areas and only rarely from more remote rural villages.
CFR – case fatality rate; DF/D–WS – dengue fever/dengue without warning signs; DHF/D+WS – dengue haemorrhagic fever/dengue with warning signs; DSS/SD – dengue shock syndrome/severe dengue.
* Based on population prediction of the Lao People’s Democratic Republic National Census 2005.
Case reporting was highest from May/June to October/November with peaks in late August or September. In 2008, cases peaked earlier in June, and in 2012 cases peaked in October. Between the years 2006 and 2009, the outbreak alert threshold was exceeded every week during May through November, but the epidemic threshold was reached for only one to two weeks at a time. In contrast, in 2010, reported dengue cases exceeded the epidemic threshold consistently from week six to week 45 (39 weeks duration) (Figure 3). Case reporting was exceptionally low and the outbreak threshold was only crossed twice in 2011. In 2012, cases exceeded the epidemic threshold for 16 weeks from week 35 onwards.
Between 2007 and 2012, a total of 323 outbreaks were notified (all causes), and dengue was suspected in 41 (13%) events (Table 2). In total, 76% (31/41) of dengue outbreak investigations included specimen collection (at least one sample) and 81% (25/31) were laboratory confirmed at NCLE. In 2010, 11 of 35 (31%) outbreaks were suspected dengue, and 3 of 7 (43%) outbreaks were confirmed. In 2012, all suspected dengue outbreaks (n = 14) led to investigations and sample submissions, with 13 of 14 outbreaks confirmed. Most outbreaks were notified through ad hoc event-based surveillance rather than via Lao EWARN.

NR – not recorded
* Cases recorded for four of nine reported outbreaks.
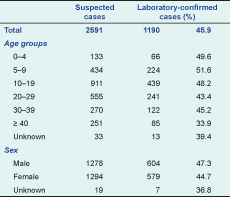
From 2000 to 2006, an average of 20 sera per year from suspected dengue cases were submitted for analysis (Table 3). These specimens comprised referrals from provincial hospitals and samples from outbreak investigations. Specimen referrals increased steadily from 2007 and 2010, reaching a total of 733 specimens in 2010, dropping in 2011 due to low case numbers and increasing again in 2012 to 852 specimens. The number of laboratory-confirmed dengue samples by age and sex aggregated from 2008 to 2012 are presented in Table 4. There was a lower proportion of laboratory confirmed dengue in the 40-years-and-older age group (33.9%, P < 0.01) compared to younger age groups (43.4–51.6%). Since the establishment of in-house molecular serotyping in 2006, a total of 798 sera have been processed by RT–PCR. All four serotypes were detected in 2008, 2009 and 2010 (Table 5). Serotype 1 was the predominant serotype detected in the period 2007–2011, and serotype 3 (n = 102/109, 94%) was the most frequent in 2012.
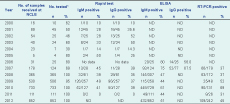
* Reflects the number of sera processed by any diagnostic test (Rapid Test, ELISA, and/or PCR).
ELISA – enzyme-linked immunosorbent assay; NCLE – National Center for Laboratory and Epidemiology; ND – not done; RT-PCR – real-time polymerase chain reaction.
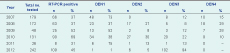
RT-PCR – real-time polymerase chain reaction.
The dengue case data from the Lao People’s Democratic Republic indicate a high and increasing burden of disease as evidenced by the annual notification rate (62–367 cases per 100 000 population), numbers of outbreak alerts, the concurrent co-circulation of all four dengue virus subtypes and the explosive nationwide epidemic in 2010 (Table 1). A trend of increasing emergence is similar to that reported from neighbouring countries; in 2010, the Lao People’s Democratic Republic had the highest notification rate in the Western Pacific Region.8
Fluctuations in severity of disease over the surveillance period, such as the significantly higher CFR in 2008, are difficult to explain. Given the changes to dengue case definitions in 2011, interpretation of trends over the surveillance period should be made with caution. Development of statistical approaches to correct for the impact of these modifications would be a useful contribution for countries with such discrepancies in national data sets. Although our finding of an excess of male suspected dengue cases in 2010 are consistent with a recent assessment of gender distribution in one province in the Lao People’s Democratic Republic,9 we found no significant difference in laboratory-confirmed cases.
Provinces with large cities and high levels of rural–urban migration regularly reported the highest case numbers. More rural and isolated provinces, however, also had higher notification rates from 2009. One outbreak in a remote village in Xayabury Province during the dry season was particularly noteworthy because the serotype was genotypically endemic DEN1, but ecological factors suggested the possibility of sylvatic transmission.10 Expansion of dengue to rural areas should be closely monitored as these populations are particularly vulnerable with poor access to health-care facilities. As seen in most dengue-endemic countries, disease transmission is highly seasonal in the Lao People’s Democratic Republic and coincides with the wet season. To date, the national case data do not suggest a clear pattern of epidemic cycles as has been found elsewhere in the Region.11,12
The data presented here suggest a trend of increased transmission and geographic expansion (Figure 2) throughout the country as has been seen across the region.8 However, the apparent dengue disease emergence may be partly explained by ascertainment bias introduced by ongoing evolution of the surveillance infrastructure. Dengue case reporting in the Lao People’s Democratic Republic has surely been influenced by national awareness and community education campaigns, changing health-seeking behaviour and improved access to telecommunications. Increased awareness of dengue was evidenced by trends in outbreak notifications (Table 2) and increases in specimen referral (Table 3). Development of the Lao EWARN system in 2008 facilitated automated tracking in real time and for the first time enabled data validation exercises and timely feedback to health offices to encourage regular reporting. However, the current surveillance system still has numerous inherent limitations including poor access to health-care facilities, clinical and laboratory misdiagnosis through confounding dengue with other diseases13,14 and underreporting of deaths due to cultural preferences for family members to die at home. Moreover, internal evaluations of the surveillance system have found inconsistent use of clinical case definitions and weekly variability in the number of sites reporting each week; there is not yet a system to link laboratory test results to case reporting nor a systematic reporting of RDT results during outbreak investigations. Molecular serotyping results for the period were likely biased towards outbreak samples as these were more frequently sampled and sequenced than routine referral samples.
The dengue surveillance system in the Lao People’s Democratic Republic has made extraordinary progress and currently meets many of the key international recommendations for surveillance and outbreak response. The outbreak alerts that are triggered regularly via Lao EWARN during epidemic years tend to overwhelm provincial and district health offices, and resources are often insufficient to verify and investigate all alerts. Hence, village outbreaks continue to be notified primarily through event-based surveillance, whereas the weekly indicator-based system provides systematic assessment of annual epidemic cycles. The NCLE, the Lao Oxford Mahosot Hospital Wellcome Trust Research Unit and Institute Pasteur have initiated systematic virological testing of dengue samples from several sentinel provinces; RDT results are now being reported from the field, the serotype/sequence database on dengue is accumulating, and a new working group has been established to coordinate analysis and interpretation of dengue data. The forthcoming analyses will assist in the critical task of designing and implementing effective preparedness and interventions strategies, including contingency plans and risk assessment schemes, and guiding policy-makers in making decisions on vaccine introduction when available.
None declared.
None.