
a Emerging Diseases Surveillance and Response. Division of Pacific Technical Support, World Health Organization, Suva, Fiji.
b Ministry of Health and Medical Services, Honiara, Solomon Islands.
c WHO Solomon Islands Office, World Health Organization, Honiara, Solomon Islands.
d Medical Laboratory. National Referral Hospital. Honiara, Solomon Islands.
e WHO Collaborating Centre for Arbovirus Reference and Research, Queensland University of Technology, Brisbane, Australia.
f Unit of Emerging Infectious Diseases. Institut Louis Malardé, Papeete, French Polynesia.
Correspondence to Francisco Nogareda (e-mail: nogaredaf@wpro.who.int).
To cite this article:
Nogareda F et al. Ongoing outbreak of dengue serotype-3 in Solomon Islands, January to May 2013. Western Pacific Surveillance and Response Journal, 2013, 4(3):28–32. doi:10.5365/wpsar.2013.4.2.013
Introduction: In January 2013, clinicians in Honiara, Solomon Islands noted several patients presenting with dengue-like illness. Serum from three cases tested positive for dengue by rapid diagnostic test. Subsequent increases in cases were reported, and the outbreak was confirmed as being dengue serotype-3 by further laboratory tests. This report describes the ongoing outbreak investigation, findings and response.
Methods: Enhanced dengue surveillance was implemented in the capital, Honiara, and in the provinces. This included training health staff on dengue case definitions, data collection and reporting. Vector surveillance was also conducted.
Results: From 3 January to 15 May 2013, 5254 cases of suspected dengue were reported (101.8 per 10 000 population), including 401 hospitalizations and six deaths. The median age of cases was 20 years (range zero to 90), and 86% were reported from Honiara. Both Aedes aegyti and Aedes albopictus were identified in Honiara. Outbreak response measures included clinical training seminars, vector control activities, implementation of diagnostic and case management protocols and a public communication campaign.
Discussion: This was the first large dengue outbreak documented in Solomon Islands. Factors that may have contributed to this outbreak include a largely susceptible population, the presence of a highly efficient dengue vector in Honiara, a high-density human population with numerous breeding sites and favourable weather conditions for mosquito proliferation. Although the number of cases has plateaued since 1 April, continued enhanced nationwide surveillance and response activities are necessary.
Solomon Islands is an archipelago located in the South Pacific comprising a double chain of 992 islands with a population of 515 870 in 2009. It is divided into nine provinces, and 80% of the population live in rural areas (Figure 1). The National Referral Hospital (NRH) is located in the capital city, Honiara. Syndromic surveillance is conducted at seven sentinel sites, four sites in Honiara and three in the provinces.

During the first week of January 2013, clinicians at NRH noted several patients presenting with dengue-like illness. Serum from three cases was positive for dengue virus (DENV) by rapid diagnostic test (RDT). Over subsequent weeks, increasing numbers of suspected and RDT-positive dengue cases were identified. On 6 March, dengue serotype-3 (DENV-3) was isolated from four patients. By 15 May, more than 5200 suspected cases had been identified. This report describes the ongoing outbreak investigation, findings and response.
During the last week of January 2013, enhanced dengue surveillance was implemented in Honiara and Guadalcanal Province health facilities and was progressively implemented in the remaining provincial hospitals over the subsequent six weeks. This comprised the training of clinical staff in case detection and notification, distribution of RDT to hospitals and the development and implementation of a database and protocol for collating and analysing the surveillance data. The dengue surveillance data were submitted weekly by health facilities to the National Surveillance and Response Unit of the Ministry of Health for analysis and dissemination.
A suspected case of dengue was defined as a patient with fever by clinical history or examination (≥ 38 °C); a negative malaria test (malaria RDT or microscopy parasite smear) plus two or more of the following symptoms: anorexia and nausea, rash, aches and pains (headache, eye pain, muscle ache or joint pain); a positive tourniquet test; leukopenia (< 4000/ml); or a dengue warning sign (abdominal pain or tenderness, persistent vomiting, mucosal bleeding, liver enlargement > 2 cm, clinical fluid accumulation, lethargy, restlessness, increase in haematocrit concurrent with rapid decrease of platelet count). Rates were calculated using the 2009 census data, which were aggregated by age (< 15, 15–24, 25–59 and 60+).
Serum was collected for RDT testing (Dengue Duo, Standard Diagnostics Inc., Kyonggi-do, Republic of Korea) from suspected cases that had warning signs or cases from areas with unknown, new or poorly characterized dengue transmission. The RDT was considered positive for dengue if it tested positive for non-structural protein 1 (NS1) and/or anti-DENV immunoglobulin M (IgM).1 Further testing by enzyme-linked immunosorbent assay (PanBIo Dengue IgM capture ELISA, Queensland, Australia) and cell culture was conducted by the World Health Organization (WHO) Collaborating Centre for Arbovirus Reference and Research in Brisbane, Australia and by reverse transcriptase polymerase chain reaction (RT–PCR) by the Institut Louis Malardé, French Polynesia.
The National Vectoborne Disease Control Programme conducted vector surveillance activities, including larval surveillance and aspiration of adult mosquitoes from February to late April across several Honiara suburbs. Adult vectors were collected using ad hoc indoor and outdoor human landing catches at peak biting times. The vector surveillance was implemented to establish the presence and distribution of dengue vectors in Honiara and other provincial capitals where dengue cases were being recorded, including Auki in Malaita Province and Gizo in Western Province.
From 3 January to 15 May 2013, there were 5254 cases of suspected dengue reported (101.8 per 10 000 population). Approximately 9% of cases (n = 401) reported in Honiara were admitted to NRH. No data was available for hospitalization rates outside the capital. Six patients died (case fatality: 0.1%).
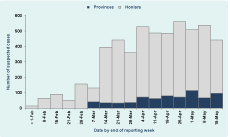
Males comprised 47% of suspected cases and the median age was 20 years (range zero to 90). Adults aged 15 to 24 and 25 to 59 years were most affected with 125 and 112 cases per 10 000 population (age-adjusted), respectively. The least affected age group was adults aged > 60 years with 41 cases per 10 000 population. Most cases (86%) were reported from Honiara (703 cases per 10 000 population), followed by Western Province and Guadalcanal Province (excluding Honiara) with 34 and 28 cases per 10 000 population, respectively (Table 1). The number of new cases reported from Honiara has been stable since 1 April 2013, while the number of suspected cases in the provinces has been increasing since the beginning of March (Figure 2).
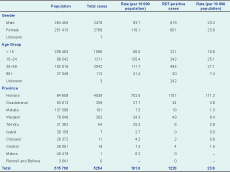
RDT – rapid diagnostic test
Sera from 3141 suspected cases were tested by RDT, and 1220 (39%) were positive. On 13 February, anti-dengue IgM was detected in four of 12 samples by ELISA testing. On 6 March 2013, cell culture from four RDT NS1-positive and IgM-negative samples isolated DENV-3. An additional 10 RDT NS1-positive samples were RT–PCR positive for DENV-3.
Targeted sampling of mosquito breeding sites in Honiara identified two receptacles positive for Aedes aegypti and 152 receptacles positive for Aedes albopictus. Dengue vector surveillance outside Honiara (rural Guadalcanal, Malaita and Gizo) identified only Aedes albopictus.
Control measures implemented by the Ministry of Health and Medical Services with WHO support included: clinical training seminars, based on WHO clinical management guidelines,2 for doctors and nurses to ensure high-quality patient care; implementation of diagnostic and case management protocols for health care professionals; vector control activities including: blanket space-spraying of Honiara and focal treatments of case house clusters with interior residual sprays, exterior residual sprays, residual treatment of breeding sites and targeted ultra-low volume fogging; and public communication campaigns including press statements, radio messages and house-to-house delivery of dengue information pamphlets, educating the public on the prevention of mosquito bites, the signs and symptoms of dengue, and promoting early health-seeking behaviour. Government of Solomon Islands declared a national clean-up day on 20 March 2013, further encouraging the public to remove, cover or destroy potential mosquito breeding sites such as old tyres, rubbish and other water–filled containers.
At the time of reporting, the DENV-3 outbreak in Solomon Islands continues. The capital city, Honiara, is the epicentre of the outbreak with almost 90% of suspected cases and where, from January to May, more than 7% of the population have met the criteria for suspected dengue and presented to a health facility. Despite a relatively low hospitalization rate of 8.6%, the strain on the health system has, and continues to be, substantial.
As dengue is a serotype-specific immunizing infection, the broad and even age distribution up to 49 years of age suggests an absence of prior DENV-3 infection – and thus susceptibility – in the majority of the population. Despite the large susceptible population, the number of new dengue cases has plateaued since April 2013. This may be due, at least in part, to the implementation of effective control measures. The normal seasonal decrease in rainfall from April to June, with the corresponding decrease in mosquito population, is also a likely contributing factor.3–5 At this time, the provinces have not experienced substantial dengue activity when compared to Honiara, which may be due to an absence of Aedes aegypti combined with lower population density in a predominantly rural versus urban environment. Aedes albopictus, which is the only dengue vector identified outside Honiara, has been implicated as an epidemic vector of dengue but usually in smouldering outbreaks characterized by limited rather than explosive transmission. Conversely, Aedes aegypti is a more efficient and effective dengue vector and is frequently implicated as the primary epidemic vector in explosive dengue outbreaks.6
The outbreak response was initiated in January after the detection of the first locally acquired cases. Subsequent response measures focused on limiting dengue transmission and minimizing progression to severe or complicated dengue. Due to the limited capacity and the lack of knowledge on dengue fever by health care professionals and the population, effective response actions were delayed, especially at the provincial level, because training was required to inform clinicians about dengue symptoms, treatment and preventive and control measures. Due to limited resources, vector and larval surveillance were aimed at determining vector presence/absence and approximating spatial distribution rather than densities.
This DENV-3 outbreak is continuing in Solomon Islands. Continued nationwide enhanced surveillance and response activities are recommended with particular attention needed at the provincial level, which is experiencing an increasing number of cases and where medical and other response capacity is limited.
None declared.
None.
The authors acknowledge the health staff of the health centres and hospitals in Solomon Islands, the medical laboratory at the National Referral Hospital in Honiara, and the National Vectorborne Disease Control Programme for their collaboration during the outbreak.