a Department of Acute Critical Care and Disaster Medicine, Tokyo Medical and Dental University, Tokyo, Japan.
b Emerging Diseases Surveillance and Response, Division of Health Security and Emergencies, World Health Organization Regional Office for the Western Pacific, Manila, Philippines.
Correspondence to Hiroto Ushizawa (e-mail: ushihi@nih.go.jp).
To cite this article:
Ushizawa H et al. Needs for disaster medicine: lessons from the field of the Great East Japan Earthquake. Western Pacific Surveillance and Response Journal, 2012, 4(1):51–55. doi:10.5365/wpsar.2012.3.4.010
Problem: The Great East Japan Earthquake, which occurred in Tohoku, Japan on 11 March 2011, was followed by a devastating tsunami and damage to nuclear power plants that resulted in radiation leakage.
Context: The medical care, equipment and communication needs of four Disaster Medical Assistance Teams (DMAT) during four missions are discussed. DMATs are medically trained mobile teams used in the acute phase of disasters.
Action: The DMATs conducted four missions in devastated areas from the day of the earthquake to day 10. The first and second missions were to triage, resuscitate and treat trauma victims in Tokyo and Miyagi, respectively. The third mission was to conduct emergency medicine and primary care in Iwate. The fourth was to assist with the evacuation and screening of inpatients with radiation exposure in Fukushima.
Outcome: Triage, resuscitation and trauma expertise and equipment were required in Missions 1 and 2. Emergency medicine in hospitals and primary care in first-aid stations and evacuation areas were required for Mission 3. In Mission 4, the DMAT assisted with evacuation by ambulances and buses and screened people for radiation exposure. Only land phones and transceivers were available for Missions 1 to 3 although they were ineffective for urgent purposes.
Discussion: These DMAT missions showed that there are new needs for DMATs in primary care, radiation screening and evacuation after the acute phase of a disaster. Alternative methods for communication infrastructure post-disaster need to be investigated with telecommunication experts.
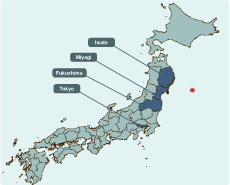
The Great East Japan Earthquake occurred at 14:46 on 11 March 2011. The centre of the earthquake was offshore of Sanriku in Miyagi Prefecture in Tohoku, Japan (Figure 1). The magnitude was 9.0 with a maximum seismic intensity of 7.0 at a depth of 24 km. A tsunami followed 15 minutes after the earthquake. Reactors at nuclear power plants were badly damaged and resulted in radiation leaking into the surrounding Fukushima Prefecture. The magnitude and duration of shaking (more than three minutes) ranked this earthquake as one of the largest earthquakes since 1990.1
* Epicentre - 38 o 6' 12" N 142o 51' 12" E (Japan Meteorological Agency)
Casualties from the Great East Japan Earthquake were typical for earthquakes followed by tsunamis with large numbers of dead and missing people but a small number of injured (dead 15 879, missing 2700, injured 6130; injury-to-death ratio was 0.4).2-4 In comparison, the 1995 Great Hanshin-Awaji Earthquake, one of the largest earthquakes in Japan without a tsunami, had 6434 deaths, three missing and 43 792 injured (injury-to-death ratio was 6.8).5 The Great East Japan Earthquake resulted in less need for trauma surgery and resuscitation and a higher need for primary care.
This paper discusses the experience in the field of members of the Tokyo Medical and Dental University Hospital (TMDUH) Disaster Medical Assistance Teams (DMATs) and concentrates particularly on medical expertise, equipment needs and operational or tactical field communication needs.
Action following any disaster requires response from a broad set of areas including public health, security, social structures, public works and engineering, education, energy supply, food and nutrition, shelter and clothing, water and sanitation, medical care, logistics and transportation and communication.6 DMATs are medically trained mobile teams used in the acute phase of disasters. They were introduced into Japan in 2005 after recognizing a gap between the capacity of conventional emergency assistance and the need for emergency medicine in the days immediately following disasters. It has been estimated that the medical assistance teams may have prevented up to 500 deaths following the Great East Japan Earthquake.7
There were more than 700 DMATs in Japan in March 2010. Between day 1 and day 12 post-earthquake, 1816 members from about 340 DMATs gathered in the devastated area.8 In this paper, the authors focus on the broadening of requirements for DMATs for medical care, logistics and transportation and communication.
Four TMDUH DMATs conducted four missions. Mission 1 was conducted in Tokyo on the day of the earthquake. Missions 2, 3 and 4 were carried out in three different prefectures of Tohoku. Miyagi is the closest prefecture to the centre of the earthquake. Iwate and Fukushima lie north of Miyagi (Figure 1). Three TMDUH DMAT members were dispatched twice to different areas.
The first TMDUH DMAT mission was to triage, resuscitate and treat trauma patients from a collapsed building in Tokyo. The DMAT left TMDUH 34 minutes after the earthquake. The collapsed building was an historic building called Kudan Kaikan where a graduation ceremony was being held. During the earthquake, the ceiling fell, and a mass casualty incident occurred with 36 casualties. After triaging, 17% were classified as severe and urgent casualties including a traumatic cardiopulmonary arrest and severe head and chest trauma, 22% as intermediate casualties and 61% as minor casualties.
While responding to Kudan Kaikan, the DMAT tried without success to communicate with TMDUH. While the mobile networks were operational, connection was not possible due to overuse of the system. Therefore, the DMAT was unable to inform the hospital of the number and the type of victims being sent there.
Mission 2 in Miyagi began the day after the earthquake and lasted to day 3. The TMDUH DMAT mission was to assist with emergency medical needs of the Sendai Medical Centre (SMC), which is 5 km from the coastline. Nine DMATs from all over Japan gathered at SMC. They rotated among four posts: severe and urgent care, intermediate care, minor care and triage. Activity was intense with casualties constantly being transferred from devastated areas. About 100 ambulances per day transferred casualties to SMC, seven times more than usual. Thirteen per cent of all casualties were severe and urgent; almost all of them were trauma patients. The majority of casualties with no need for admission had mild hypothermia. DMATs needed resuscitation and trauma sets and blankets.
During these two days, communication was limited to working land phones and transceivers to connect with paramedics operating in the devastated areas. DMATs collected information only through face-to-face meetings with paramedics from the affected areas. Therefore, DMATs were unable to know the casualty numbers and to prepare for individual casualty needs before their arrival.
Mission 3 began approximately one week after the earthquake, and although this was not originally designated as an activity of DMATs, they were deployed to Iwate. The mission was to provide emergency medicine and primary care. The TMDUH DMAT assisted Ofunato Prefectural Hospital (OPH), five first-aid stations and an evacuation area. OPH lies only 1.5 km from the coastline.
At this hospital, only 3% of patients required severe and urgent care, 50% required intermediate medical care and 47% required minor medical care.
The DMAT made rounds to five first-aid stations and an evacuation area near the coastline. Most patients presented with mild respiratory infection; there were few direct disaster-related presentations. Medical expertise and equipment were needed to treat emergency and primary care patients. Ambulances were needed 2.6 times more than usual because other hospitals in the area were destroyed.
Despite no urgent need for communication in this mission, the DMATs communication options and capabilities were still limited. The satellite phone worked in OPH, but it took about 10 minutes to connect to service and was therefore not used for urgent situations.
Mission 4 began nine days after the earthquake in Fukushima. The coastal area in Fukushima was polluted by radiation following damage to a nuclear power plant. The TMDUH DMAT and other DMATs coordinated with the Emergency Headquarters of Radiation Exposure which comprised the Nuclear and Industrial Safety Agency and the National Institute of Radiological Sciences at the Fukushima Prefectural Government.
The TMDUH DMAT screened inpatients in the hospitals and health care facilities for radiation exposure and evacuated casualties from the radiation-affected area. Elderly and disabled patients in hospitals and nursing homes were transferred to screening points at a high school. Members of the DMAT wore personal protective equipment and screened the patients using dose-metres to detect the amount of radiation exposure. None of the patients' exposure level was higher than the baseline.
At this point in time, almost all communication methods were available and operable.
The experiences of the TMDUH DMATs on the four missions varied with regards to medical expertise, equipment and communication (Table 1). The DMATs' medical training and experience in trauma and emergency care was absolutely necessary for the first two missions. The equipment used was mainly for trauma-associated cases. A large number of ambulances and basic supplies such as blankets for hypothermia were needed.
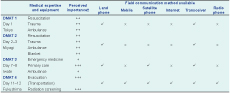
* TMDUH DMAT - Tokyo Medical and Dental University Hospital Disaster Medical Assistance Team
+ Perceived importance of medical expertise and equipment ranked by TMDUH DMAT from + to +++
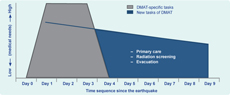
New functions were required of DMATs during Missions 3 and 4. DMATs, who are trained to be flexible by assisting in various medical situations, were deployed for primary care surge capacity and in the unusual circumstances of supporting mass screening and transportation of patients from radiation-affected areas (Figure 2).
A significant difficulty arose from the lack of adequate operational communication. While phones and communication equipment were available, communication links did not function due to heavy use by other citizens. This lack of communication made it difficult to get credible information from the field about the devastated areas, and it was necessary to allow greater time for handover of the casualties through face-to-face communication with paramedics once the ambulances reached the hospitals.
The two main lessons learnt by TMDUH DMATs were those associated with field communication and that new tasks were required for this specific response. From day 1 to day 8, TMDUH DMATs suffered poor communication capability, similar to that of other DMATs.9 As a result, the most credible method for collecting medical information about the patients being transported to hospitals was by talking with paramedics on arrival from the affected areas. Improved and alternative methods for communication infrastructure post-disaster have been suggested,10 and DMATs wish to work with telecommunication experts in this development, including the utilization of satellite phones. The main benefit of satellite phones is that they can be used independently of busy phone lines or Internet connections and mobiles. However, this experience showed that a weakness of satellite phones is the slowness of the connection between two areas. Technological innovation will make satellite phones more useful tools. During the World Trade Center attack in 2001, "the lack of communication method probably resulted in more problems than all other factors combined."11 Many stakeholders have a serious interest in improving communication during disasters.
Through the TMDUH DMAT experience, new additional duties for DMAT operations were recognized. After the acute phase of a disaster, surge capacity in the devastated area was needed for primary care, radiation screening and evacuation (Figure 2). In general, medical services are required immediately following a disaster; this need then decreases day by day. During the earthquake response, DMATs focused on trauma treatment and resuscitation from day one to day three. In previous events, TMDUH DMATs did not participate in further medical support. However in this event DMATs were used for new needs in disaster medicine - a novel outcome.
There are some limitations in this paper. As it reflects the experience of only TMDUH DMATs following the Great East Japan Earthquake, the perceived importance of expertise, equipment and operational communication may not be representative of all DMATs. The number of patients to whom we provided medical care in Missions 2 to 4 could not be accurately counted. However, this firsthand experience has value as it identifies significant communication issues and expanded roles for DMATs in the future.
In conclusion, DMATs must be ready to lessen preventable deaths and further injury during the acute phase of an emergency response. As this paper and others show, there are additional needs for DMATs in primary care, radiation screening and evacuation.12,13 DMATs should be prepared to practise primary care and address radiation as indispensable knowledge in the future. DMAT training courses should include lectures, simulated training and examination on primary care and radiation issues. The experience of the TMDUH DMATs shows that there is a need to broaden both the professional flexibility of DMAT members and communication methods during disaster responses.
None declared.
None.