a Field Epidemiology Training Programme, Hong Kong, People’s Republic of China.
b Department of Health, Hong Kong, People’s Republic of China.
c Hospital Authority, Hong Kong, People’s Republic of China.
Correspondence to Tsz-sum Lam (e-mail: mo_fetp1@dh.gov.hk).
To cite this article:
Lam T et al. Bacille-Calmette-Guérin vaccine-associated suppurative lymphadenitis in Hong Kong (China), 2004 to 2012. Western Pacific Surveillance and Response Journal, 2013, 4(1):39–40. doi:10.5365/wpsar.2013.4.1.001
We note with interest the theme of “Tubercousis (TB)” for this issue of the Western Pacific Surveillance and Response Journal and wish to share our experiences in investigating suppurative lymphadenitis as a result of the Bacille-Calmette-Guérin (BCG) vaccine in Hong Kong (China).
The TB notification rate in Hong Kong (China) has been decreasing in the past 50 years from a peak of 697 per 100 000 in 1952 to 72.5 per 100 000 in 2010. The number of TB notifications in Hong Kong (China) in 2010 was 5093.1
The BCG vaccine for the prevention of TB was developed almost 100 years ago and use of the vaccine commenced in Hong Kong (China) in 1952. The vaccine protects children against severe forms of TB such as TB meningitis and miliary TB.2 In Hong Kong (China) we use freeze-dried BCG (Statens Serum Institut of Denmark, Copenhagen 1331 strain) by intradermal method. Orignally, vaccination was offered to all newborns infants and again for primary schoolchildren; however, in September 2000, the BCG revaccination programme for primary schoolchildren was stopped.1 Adverse effects of BCG vaccination have been reported in many countries of the world. Suppurative lymphadenitis is a known reaction with a background rate of one to 10 per 10 000 doses globally.3 In 2010 in Hong Kong (China), more than 99% of newborn infants were given direct BCG vaccination at birth.1
To assess the trend of hospitalized BCG lymphadenopathy in recent years, we reviewed records of patients hospitalized between 1 January 2004 and 31 December 2012 with relevant ICD-9 code diagnoses of BCG-related adverse effects and lymphadenopathy from all public hospitals in Hong Kong (China). Public hospitals account for around 80% of secondary and tertiary care in Hong Kong (China).4 We traced relevant demographics and clinical information of every patient through review of clinical records and interviews with patients’ parents or caretakers.
We identified 109 patients with suppurative BCG lymphadenitis. Two patients hospitalized in 2004 received BCG in 2003. There were 79 boys (72%) and 30 girls with ages ranging from 14 days to 23 months old (median five months). The period between BCG vaccination and symptom onset (discovered by caretakers) ranged from 0.5 to 18.5 months (median 3.4 months). Most (94 [86%]) presented with left axillary lymphadenopathy, three supraclavicular, three infraclavicular, two clavicular, one cervical and six with left axillary and other regional lymphadenopathy. Half (56 [51%]) were managed by needle aspiration (initial management recommended by local paediatricians5), 21 by incision and drainage, 10 by excision and 22 by observation with follow-up.
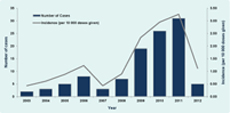
The number of suppurative BCG lymphadenitis patients increased from three to 31 in the vaccination years 2007 to 2011 (Figure 1). Although the incidence remains in line with the World Health Organization estimation (one to 10 per 10 000 doses), there was an increase in incidence of suppurative BCG lymphadenitis from 0.43 to 3.26 per 10 000 doses in vaccination years 2007 to 2011. BCG has been worthwhile for the decrease of TB notification rates in Hong Kong (China) since 1952. We recommend setting up special surveillance to monitor trends of suppurative BCG lymphadenitis in Hong Kong (China).
* The number of cases and incidence for 2012 was lower than the preceding three years. This may be due to incomplete hospital data as we reviewed the data on 3 January 2013. On the other hand, the median latency period between BCG vaccination and symptom onset was around three months; those vaccinated in 2012 may be hospitalized in 2013.
None declared.
None.