a National Center for Communicable Diseases, Ulaanbaatar, Mongolia.
b Mongolian Field Epidemiology Training Programme, Ministry of Health, Ulaanbaatar, Mongolia.
c World Health Organization Representative Office in Mongolia, Ulaanbaatar, Mongolia.
Correspondence to Jantsansengeegiin Baigalmaa (e-mail: j_baigalmaa@yahoo.com).
To cite this article:
Jantsansengeegiin B et al. Increasing syphilis notifications in Mongolia: results from national surveillance for 2001–2011. Western Pacific Surveillance and Response Journal, 2012, 3(4):83–90. doi:10.5365/wpsar.2012.3.2.008
Background: In Western Pacific Region countries, sexually transmitted infections (STI) rates vary but are considered high. In Mongolia, syphilis incidence has increased between 2001 and 2011; therefore, the objective of this study was to describe the epidemiology of syphilis in Mongolia to provide evidence for prevention and control activities.
Methods: A retrospective analysis of syphilis was conducted using STI data from the passive surveillance system. This included demographic and clinical information and laboratory test results. In addition, a test for the trend of syphilis notification rates over time was conducted.
Results: Syphilis notification rates increased by twofold from 71 per 100 000 in 2001 to 152 per 100 000 in 2011 (P < 0.006), and there were significant differences observed between the capital city and the province rates over time (P = 0.011). Generally, notification rates among females were significantly higher than males (P < 0.001) except that male rates increased to 185 per 100 000, higher than female rates of 179 per 100 000 in 2009. The increase of notifications of latent syphilis for males (P < 0.009) and females (P < 0.006) was significant.
Discussion: This is the first analysis of the overall situation of syphilis in Mongolia, and although the years with the largest number of cases corresponded to large-scale screening programmes, we observed a significant increase in syphilis notification rates over time. These results will be useful for evidence-based prevention and control activities such as awareness campaigns for young adults.
Sexually transmitted infections (STI) are a major public health concern. The World Health Organization (WHO) estimates that annually more than 448 million new episodes of curable STI, which include syphilis, chlamydia, gonorrhea and trichomoniasis, occur throughout the world.1 The majority of infections occur in south and south-eastern Asia, followed by sub-Saharan Africa, Latin America and the Caribbean.2
In WHO Western Pacific Region countries, STI rates vary but are generally considered high. The latest data from China showed that syphilis, which was considered controlled, has resurged in the last decade.3 In addition, a fourfold rise in gonorrhoea, chlamydia, genital herpes and genital warts was observed in China between 1990 and 2000. Similar trends have been observed in Malaysia.4 Surveys in Pacific island countries show a prevalence of syphilis of 0.3%.5 A nationwide cross-sectional study conducted in 2008 showed that among 2000 antenatal care attendees in Mongolia, 25.5% had at least one STI.6
According to the AIDS and STI surveillance department of the National Center for Communicable Diseases (NCCD), STI represented about one third of all infectious diseases reported in Mongolia between 2001 and 2010. Syphilis, gonorrhea and trichomoniasis are the most frequently reported STI, and the syphilis rate has increased between 2001 and 2011.
Therefore, for the first time in Mongolia, we aimed to describe the epidemiology of syphilis cases reported to the national STI surveillance system.
This paper is a retrospective analysis of syphilis cases reported to the national STI surveillance department in Mongolia for the period 2001 to 2011.
In Mongolia, STI care and services are provided at three levels of health care nationwide. Primary level STI care is provided through 580 family group practices and primary health care clinics, secondary level care is provided through 29 provincial and capital city district hospitals and specialized or tertiary care is provided at the NCCD.7 Due to the lack of laboratory capacity to diagnose STI at the primary health care level, syndromic diagnosis and treatment of STI was introduced in 2001.7 In 2008, in response to the high rate of congenital syphilis in the country, all clinics in eight provinces and six districts of the capital city established testing capacity for STI, including syphilis, at all programme sites (personal communication with Dr Ch Erdenechimeg, STI and AIDS Department, NCCD).
Detection and confirmatory syphilis serologic testing (rapid plasma reagen [RPR] test, Treponema pallidum haemagglutination assay [TPHA], enzyme-linked immunosorbent assay [ELISA]) are conducted at the secondary level8 and at the STI diagnostic laboratory of the NCCD.7 The latter is the national reference laboratory, and 10% of all tests from secondary laboratories are sent on a quarterly basis to the reference laboratory for confirmation and quality assurance. Quality assurance of the STI laboratory of the NCCD is conducted at the Australian serologic reference laboratory in Sydney, Australia. Syphilis test quality assurance was 100% in 2011.
According to the International Classification of Diseases–10,9 syphilis comprises two disease phases: early and late. Early syphilis is then categorized into primary, secondary and early latent syphilis; late syphilis is grouped into tertiary and late latent syphilis. Primary and secondary syphilis manifest with clinical symptoms after approximately four months of infection and are considered as new infection. Latent syphilis is an asymptomatic infection identified through serological testing and is diagnosed within or after two years of infection.
In Mongolia, at the primary STI care level, syndromic cases of primary syphilis with an obvious clinical symptom (classic chancre) are reported to the surveillance system; at the secondary and tertiary STI care levels, all cases require laboratory confirmation by RPR, TPHA or ELISA.
STI surveillance in Mongolia is a passive surveillance system. National STI surveillance and statistical data are collected from all levels of STI care and services and reported to the AIDS and STI surveillance department of the NCCD. STI care providers fill out STI outpatient cards and then send the reports to the next level of STI care. At the secondary level, the reports are summarized for the number of STI client visits, number of patients diagnosed with STI, laboratory confirmation and some contact tracing information. It is compulsory that the 21 provincial health departments and eight districts (except one, where they do not provide STI care and services) of the capital city send the reports to the AIDS and STI department of the NCCD on a monthly basis. STI surveillance and statistical data are kept and managed at the NCCD, and basic analysis is conducted on an annual basis for national statistical reporting. Case data collected include identification, social and geographic information, laboratory test results and contact tracing information.
We analysed all syphilis cases reported to the STI surveillance system from 2001 to 2011. The denominator for calculating syphilis rates was based on the 2001 to 2011 population data and estimated per 100 000 population. We conducted nonparametric trend tests across calendar-years to test for secular trends in syphilis notification rates over time.10 Trend analyses were performed using STATA. The difference between sex and geographic distribution was tested using the chi-squared test in OpenEpi.
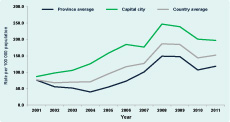
The syphilis notification rate increased twofold from 71 per 100 000 to 152 per 100 000 between 2001 and 2011. The rate was stable between 2001 and 2004; however, it began to increase after 2005, peaking in 2008 with a rate of 188 per 100 000. In 2010, a decrease in syphilis notifications was observed at 144 per 100 000 population, but the rate increased again to 152 per 100 000 in 2011 (Figure 1). Trend tests by year showed that this increase was statistically significant (P = 0.006).
Similar to the total syphilis notification rate, the notification rate of latent syphilis increased from 2005, peaking in 2008 at 134 cases per 100 000; this increase was statistically significant (P = 0.009). Primary and secondary syphilis rates remained at relatively constant levels until they peaked in 2009 with a notification rate of 27 and 49 cases per 100 000, respectively (Figure 2).

The number of serologic tests conducted for syphilis increased from 2001 and peaked in 2008 and 2009. As the number of tests performed increased, syphilis notifications, including latent syphilis notifications, also increased (Figure 3).The proportion of positive tests ranged from 1–1.5 per 100 tests between 2001 to 2011 with no statistically significant difference overall (P = 0.05). The highest proportion of positive tests (1.5%) was observed in 2007, a year in which relatively few tests were performed. The greatest number of tests were performed in 2009 and 2011 during which the proportion of positive tests was lower than 2007 and 2008 (Figure 4).
Syphilis notification rates in the capital city (Ulaanbaatar) were continuously higher than province averages over the study period, although both showed the same pattern as the total notification rates (Figure 5). There was a significant increase over time for both the capital city (P = 0.004) and province average (P = 0.023). The difference between provinces and the capital city was also statistically significant (P = 0.011).
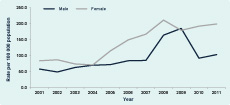
Notification rates were higher among females than males in the period 2001 to 2008; in 2009, the male notification rate was slightly higher (185 per 100 000 compared with 179 per 100 000). In 2010, the female notification rate was more than twice as high as the male rate, increasing slightly from 2009. Overall, there was a significant difference between male and female syphilis notification rates (P < 0.001) (Figure 6).
Syphilis notification rates were highest among the sexually active and reproductive age group of 20 to 39 years. In addition, notification rates of syphilis consistently increased for young people aged 15 to 19 years and 20 to 24 years over the study period (Table 1).
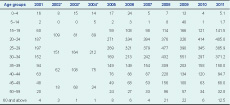
* Data of some age groups were combined in the surveillance during the period 2002 to 2004.
Overall, pregnant women comprised approximately one third of reported syphilis cases. The year 2005 had the highest proportion of syphilis notifications in pregnant women at 80% of all female syphilis cases. In 2008, the year with the highest number of syphilis notifications, pregnant women comprised 40% of female cases.
Notification rates of primary and secondary syphilis combined for females were generally higher than the rates for males between 2001 and 2009. In 2010, the notification rates decreased by half for males from 79 per 100 000 in 2009 to 35 cases per 100 000. Female rates remained the same. Tests for trends for primary and secondary syphilis combined in males (P < 0.3) and females (P < 0.1) demonstrated no significant change (Figure 7).
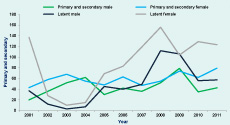
Latent syphilis notification rates in females were typically higher between 2001 and 2011 compared with males, except for 2009 when where the rates were similar (104 per 100 000 and 106 per 100 000, respectively). In 2010 and 2011, latent syphilis notification rates were more than twice as high for females (129 per 100 000 and 123 per 100 000) than for males (56 per 100 000 and 57 per 100 000). Latent syphilis both in males (P < 0.009) and females (P < 0.006) demonstrated a significant increase over time (Figure 7).
We observed a consistent increase in syphilis notifications in Mongolia from 2001, peaking in 2008 and 2009. The “Healthy Mongolian” health screening campaign organized in 2008 and 2009 provided free medical examinations including testing for syphilis (personal communication with Dr Ch Erdenechimeg, STI and AIDS Department, NCCD). Detection of cases during this screening may have contributed to the observed peak of syphilis notification rates in 2008 and 2009. There were higher female syphilis notification rates overall and difference in notifications between the capital city and the provinces. Latent syphilis in both males and females also significantly increased during the observation period, similar to the increase observed for all syphilis notifications.
The significantly higher notification rates of females compared to males could be due to detection during medical examinations required for antenatal care. As latent syphilis is only detected through diagnostic tests after two years or more of infection,8,9 there was a higher detection rate of latent male and female syphilis in the screening years, and the increase in proportions of non-pregnant women with syphilis in screening years suggest that there could be many undiagnosed syphilis cases among the population.
Syphilis notification rates were higher in Ulaanbaatar city compared to the provincial average. This may be related to the high population density,10 a large sexually active population (including students and people of working age12) and a high concentration of risk groups including sex workers. It could also be due to the differences in use and access of health services including testing.
This analysis used secondary data collected from all levels of STI care and services in the surveillance system. The accuracy of secondary data is often not known. There can be overlap in the number of cases reported or missing data in some age groups. In this study, some cases of syphilis may have been reported more than once due to the complexity of differentiating between new and previous infections. There may also have been underreporting or misreporting of syphilis cases by some provinces, differences in laboratory testing and the quality of reports from health facilities. Also, STI cases receiving health care services in private clinics are not reported to the national surveillance system and potentially could lead to an underestimation in this analysis.
Despite of these limitations, this is the first analysis of syphilis notifications in Mongolia between 2001 and 2011, and these results will be used for future comparisons. Identifying the target population for screening programmes could offer an effective public health intervention for prevention and control among the population. Knowledge and awareness-raising campaigns targeted to those aged 15–24 years of age is recommended.
None declared.
None.