a US Centers for Disease Control and Prevention, Global AIDS Program - China office, Beijing, China.
b Division of Global HIV and AIDS, Centers for Disease Control and Prevention, Atlanta, United States of America.
c HIV Department, World Health Organization, Beijing, China.
d The Joint United Nations Programme on HIV/AIDS, Beijing, China.
e Representative Office, World Health Organization, Viet Nam.
f Division of Strategic Information and Planning, HIV Department, World Health Organization, Geneva, Switzerland.
Correspondence to Marc Bulterys (e-mail: zbe2@cdc.gov).
To cite this article:
Lin W et al. Is the HIV sentinel surveillance system adequate in China? Findings from an evaluation of the national HIV sentinel surveillance system. Western Pacific Surveillance and Response Journal, 2012, 3(4):61–68. doi:10.5365/wpsar.2012.3.3.004
Background: An external evaluation was conducted to assess the performance of the national HIV sentinel surveillance system (HSS), identify operational challenges at national and local levels and provide recommendations for improvement.
Methods: The United States Centers for Disease Control and Prevention’s (CDC) Updated Guidelines for Evaluating Public Health Surveillance Systems were followed to assess the key attributes of HSS. Comprehensive assessment activities were conducted, including: using a detailed checklist to review surveillance guidelines, protocols and relevant documents; conducting self-administered, anonymous surveys with 286 local China CDC staff; and carrying out field observations in 32 sentinel sites in four provinces.
Results: China has built an extensive HSS with 1888 sentinel sites to monitor HIV epidemic trends by population groups over time. The strengths of HSS lie in its flexibility, simplicity, usefulness and increase in coverage in locations and populations. With its rapid expansion in 2010, HSS faces challenges in maintaining acceptability, timeliness, data quality, representativeness and sustainability.
Recommendations: Implementation of the national guidelines should be standardized by strengthening training, monitoring and supervision of all staff involved, including community-based organizations. National surveillance guidelines need to be revised to strengthen data quality and representativeness, particularly to include specific instructions on HIV testing result provision, collection of identifying information, sample size and sampling methods particularly for men who have sex with men (MSM), collection of refusal information, and data interpretation. Sustainability of China’s HSS could be strengthened by applying locally tailored surveillance strategies, strengthening coordination and cooperation among government agencies and ensuring financial and human resources.
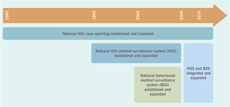
China’s first AIDS case was diagnosed in 1985.1 In 2011, the estimated number of people living with HIV/AIDS was 780 000 (620 000–940 000), of whom 48 000 (41 000–54 000) were newly infected.2 Although the overall national HIV prevalence remained low at 0.058% in 2011, the epidemic was highly concentrated in Southwestern China and Xinjiang autonomous region among key populations including injecting drug users (IDU), female sex workers (FSW) and their clients and more recently, men who have sex with men (MSM).2,3 Sexual contact was the primary transmission mode, accounting for 68% of newly reported HIV/AIDS cases in 2010.3 A dramatic increase in the epidemic was seen among MSM, which represented 29% of estimated new infections in 2011 compared to 12% in 2007.2,4 In contrast, the proportion of new infections among IDU decreased from 42% in 2007 to 18% in 2011.2,4
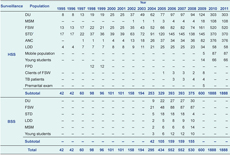
In response to the HIV epidemic, the Chinese government built a comprehensive surveillance system, which included the national HIV sentinel surveillance system (HSS), HIV/AIDS case reporting system, and special epidemiologic surveys.5–8 Before 1995, the national HIV surveillance was primarily based on a passive HIV/AIDS case reporting system in which doctors were obligated to report all diagnosed HIV/AIDS cases, with more detailed information on disease burden and high risk behaviours among specific subgroups obtained from local epidemiologic investigations and provincial HIV sentinel surveillance sites.5–8 In 1995, HSS was established at 42 sites. This system comprised routine cross-sectional surveys on risk behaviours and sero-testing of participants targeted in four population groups – drug users (DU) of which about 60% were IDU, FSW, sexually transmitted infections (STI) clinic attendees and long-distance truck drivers (LDD). More national sites were added based on need.
In 2004, an independent national behavioural sentinel surveillance system (BSS), which included a more detailed behavioural questionnaire was established. In 2009, both systems were integrated under a national standardized protocol. Most of the provincial sentinel surveillance sites were also incorporated into the national HSS. In 2010, the number of national sentinel sites expanded from 600 to 1888, targeting eight groups (DU, FSW, MSM, male STI clinic attendees, LDD, antenatal care [ANC] clinic attendees, young college students and male migrant workers) (Table 1, Figure 1).
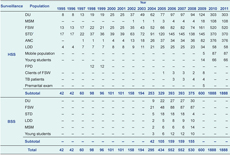
BSS – behavioural sentinel surveillance; HSS – HIV sentinel surveillance; DU – drug users; FSW – female sex workers; STI – sexually transmitted infections clinic attendees; LDD – long-distance truck drivers; ANC – antenatal care clinic attendees; FPD – former plasma donors; MSM – men who have sex with men.
* Female outpatients recruited before 2009, male outpatients recruited from 1995 to 2011.
Although several evaluations of China’s surveillance system have been conducted,9,10 the national HSS has not been evaluated since BSS started in 2004. We therefore conducted an external evaluation of HSS to assess its performance, identify operational challenges and provide recommendations to improve its performance.
The evaluation followed the United States Centers for Disease Control and Prevention’s (CDC) Updated Guidelines for Evaluating Public Health Surveillance Systems,11 focusing on assessing the attributes of the system, including usefulness, simplicity, flexibility, data quality, acceptability, representativeness, timeliness and stability.
From May to June 2011, we reviewed HSS guidelines and protocols using a detailed checklist to assess site selection criteria, sampling methods, survey contents, data collection and reporting and data analysis and use.
We conducted a self-administered and anonymous survey with 286 staff from 263 local Chinese Centers for Disease Control and Prevention (C-CDC) in 23 provinces on financial and human resources used for HSS, establishment of provincial sentinel surveillance, staffing and HSS supervision.
We conducted 32 site visits in Shandong, Jiangxi and Guizhou Provinces and Chongqing City which covered all but the male migrant worker sentinel group. We made direct observations of data collection and laboratory specimen handling; held focus group discussions; and conducted semi-structured interviews with over 100 key stakeholders including public health officials, C-CDC and laboratory staff at national and subnational levels who were involved in HSS and responsible for generating and receiving reports. Verbal informed consent was obtained and participation was voluntary. We assessed data quality by cross-checking 5% of the 2010 surveillance questionnaires against the electronic database during the field visits. Institutional Review Board review was waived.
The national HSS aims to monitor HIV prevalence and risk behaviours among targeted populations, to provide data for HIV/AIDS estimation and projection and to guide the development and impact assessment of HIV prevention and control strategies. The surveillance system comprises routine surveys of targeted populations covering demographics, detailed risk behaviours and sero-testing for HIV, syphilis and hepatitis C virus.
Site selection is based on the cumulative reported number of HIV/AIDS cases in the region, associated risk factors, local needs for HIV/AIDS prevention and intervention and local surveillance capacity. If HIV prevalence is over 5% for a high-risk population (DU, MSM, FSW and STI clinic attendees), local C-CDCs are required to establish sentinel sites targeting the general population (young students and pregnant women). If the HIV epidemic is low or uncharacterized, C-CDCs are required to establish sentinel sites targeting high-risk populations and focus populations (LDD and male migrant workers). In 2010, a total of 1888 national sites were established in 31 provinces (Table 1).
From 1995 to 2004, the HSS survey was carried out semi-annually (April to June and October to December) and from 2005, annually from April to June. In 2009, sample size requirements changed from 400 to 800 for young students and from 250 to 400 for all other populations. However, if the HIV prevalence of one target population was over 10% in the previous year, the sample size was reduced to 250.
DU are sampled in communities (snowball sampling) or detention/detoxification centres. FSW are sampled at venues (stratified sampling) or detention centres. The minimum number of low-fee and medium-fee FSW surveyed is set at 10% and 40% of the total sample size, respectively. MSM are sampled at venues (stratified snowball sampling) or through the Internet or social networks. ANC and STI clinic attendees, male migrant workers and LDD are enrolled using consecutive sampling. Young students are sampled from colleges using multistage clustered sampling method.
For the sero-testing component of HSS, provinces choose either unlinked anonymous testing (UAT)12 or linked confidential testing (LCT).12 Pre- and post-test counselling are administered and HIV testing using enzyme-linked immunosorbent assay (ELISA) and HSS-specific HIV sero-testing kits for quality control are performed at certified local C-CDC or hospital laboratories according to national HIV testing guidelines. If LCT is employed, the individual’s national identification number is collected when blood is drawn for confirmatory testing.
Local C-CDC offices are responsible for uploading data into the web-based HSS. Each provincial C-CDC conducts the surveys, submits a report to the provincial health bureau and the National Center for AIDS/STD Control and Prevention (NCAIDS) and also provides feedback to lower-level C-CDCs and facilities that carried out the surveys. NCAIDS provides feedback to provinces at the annual national HSS conference.
NCAIDS trains staff at all C-CDC levels annually and conducts annual field supervision in approximately 10% of surveillance sites in 10 provinces.
HSS has shown flexibility in adapting to changing needs over time, such as adding new population groups and questions, incorporating behavioural surveillance and changing the frequency of surveillance rounds from semi-annual to annual.
Data collection, analysis and reporting are standardized. Data entry uses an electronic online system,13 making national-level analysis and subnational comparisons easier.
Since 2002, HSS data have been used for assessing national and provincial HIV prevalence trends over time2,14–16 (Figure 2), generating national biennial HIV estimates,2,4 and monitoring and evaluating the national HIV/AIDS action plans (2006–2010 and 2011–2015) and programme planning at national and provincial levels.14,15HSS has been a major source of data for China’s Universal Access and the United Nations General Assembly Special Session (UNGASS) country progress report.16 From this perspective, HSS is useful.
DU – drug users; FSW – female sex workers; STI – sexually transmitted infections clinic attendees; ANC – antenatal care clinic attendees; MSM – men who have sex with men.
However, there are some issues with HSS that reduce its usefulness. Young student sites provide very limited information. There were no HIV infections detected and low reporting of risk behaviours at three sites that were visited. Also, although data analysis and use at the national and provincial levels are generally good, there are gaps in comprehensive analysis using multiple data sources, including surveillance, prevention and treatment programmatic data. Staff at prefecture and county levels have limited competence to analyse and use data.
The number of staff dedicated to HSS was very limited at provincial and lower levels, and the staff turnover rate was high in provinces with low HIV epidemics. Of 263 C-CDCs surveyed, 218 (83%) received supervision visits from national and/or provincial C-CDCs in 2010 compared to 162 (62%) in 2008, suggesting that oversight of HSS by national and provincial staff has been strengthened since 2008.
In 2011, 12 000 Renminbi (US $1850) was allocated per sentinel site. However this amount was insufficient for sites surveying MSM and FSW as it did not include costs for mobilization, advocacy, training and supervision.
A basic standardized data analysis and reporting plan is used uniformly nationwide, enabling timely reporting to provincial and national levels. However, mandatory reporting of HIV test results using LCT is not as timely. In 10 sites visited, specimens were held for batch testing until late in the surveillance period and results were reported to implementing facilities and individuals as much as three months after blood draw, delaying prompt care and treatment, especially for HIV-infected pregnant women.
Collaboration within C-CDC agencies is high; however, there is lack of support from stakeholders. Hospitals and clinics with large patient flow are often reluctant to conduct surveys. At some school sites, HSS surveys are conducted among student volunteers, which may underestimate risk behaviours of this group. Acceptability of HSS among FSW is variable, waning during and soon after police crackdowns of FSW activity.
Overall, 99.6% (1881/1888) of HSS sites collected data in 2010 and over 80% (1520/1881) of the sites achieved sufficient sample size. Data were accurately reported with mistakes (data missing or discrepancies between questionnaires and database) found in only six (1%) electronic entries compared with the questionnaires.
However, compliance with the national protocol at local levels needs to be promoted. Collection of personal identifying information was observed, which could have a significant impact on the acceptability of HSS and the accuracy of information reported by participants, particularly for populations involved in illicit activities or subject to stigma, such as DU, FSW and MSM.
In clinical settings, laboratory technicians had limited knowledge of national HSS testing guidelines. Use of non-surveillance specific sero-testing kits was noted at two sites and inappropriate storage of test kits were reported at a provincial C-CDC where the kits were distributed.
Lack of information reported on refusal logs hindered our assessment of overall representativeness. However, we observed that convenience sampling of MSM through the Internet or social networks was frequently used, leading to oversampling of those who were younger, interested in HIV testing, with large social networks or access to the internet. IDU were frequently surveyed in detention or detoxification centres due to easier implementation, even though they did not necessarily represent drug users in the community. At some sites, STI clinic attendees were selected based on the physician’s judgment of their likelihood to be at risk and the physician’s patient load. Patients seen during peak hours were less likely to be surveyed than those seen at other times. Some pregnant women were selected at the time of delivery, allowing duplication and exclusion of known HIV-positive pregnant women who might have terminated their pregnancies.
China has built an extensive sentinel surveillance system to monitor HIV epidemic trends by population group over time. The strengths of China’s HSS lie in its flexibility and relative simplicity. With its rapid expansion in 2010, however, HSS faces challenges in maintaining data quality, representativeness and sustainability. Addressing these challenges will allow HSS to provide accurate information for monitoring HIV transmission in the country.
This evaluation is subject to several limitations. We did not evaluate the HIV/AIDS case reporting system or special epidemiologic survey components of the HIV/AIDS surveillance system. Given the large variation in HIV epidemic patterns and local capacities, data from the 32 sites visited may not accurately reflect the performance of HSS as a whole. Staff interviewed were selected for convenience and all information was self-reported. We did not interview HSS participants to determine the acceptance of surveillance activities and representativeness of HSS.
HSS in China can be further strengthened to improve its sustainability, acceptability, data quality and representativeness. To strengthen sustainability, NCAIDS could consider estimating financial and human resources on real needs and prioritizing high HIV epidemic provinces. Strengthened coordination and cooperation among government agencies should also be considered to improve recruitment and facilitate information sharing. Different surveillance strategies should be used for high and low HIV epidemic areas. For example, in low HIV epidemic areas, NCAIDS may consider focusing on high-risk populations, conducting surveillance rounds every two years for population groups with stable HIV prevalence and dropping young students as they are not a good sentinel population for early warning of HIV epidemics. Data from voluntary blood banks may be considered for monitoring HIV infections among low-risk populations. In high HIV epidemic areas, in addition to sentinel surveillance among high-risk populations, routine HIV testing data at ANC, STI and methadone maintenance treatment clinics could also be used for surveillance purposes. This will require scaling up provider-initiated HIV testing and counselling, and improving HIV testing, data quality and collaboration between C-CDCs and clinical facilities. These improvements will lessen the burden of sentinel surveillance on C-CDC staff who are already overloaded, and hence strengthen the acceptability, sustainability and quality of such a huge surveillance system.
To strengthen data quality and representativeness, we recommend NCAIDS consider revising national surveillance guidelines to include specific instructions on HIV testing and timely test result provision (using LCT12 instead of UAT so that the participants are able to receive their test results), collection of identifying information, sample size and sampling methods particularly for MSM, collection of refusal information and data interpretation in the surveillance report. Strengthening training, monitoring and supervision of all staff involved in HSS should also be considered. Trainings for laboratory technicians should cover specific requirements for HSS testing, which are different from HIV diagnosis requirements. Continuing to strengthen data analysis and utilization is equally important. In addition to refresher trainings on sentinel surveillance for C-CDC staff, basic epidemiology and statistical analysis training should be offered at local levels to strengthen the use of surveillance data. Finally, evaluation of the HIV/AIDS case reporting system and special surveys should be considered to improve the understanding of the performance of the overall HIV surveillance system in China.
None declared.
United States CDC Global AIDS Program (3 U2G PS001188) and World Health Organization (PO200334675, PO200431207).
We would like to express our most sincere acknowledgement to the staff at NCAIDS, local C-CDCs and implementing partners for their dedication and hard work in conducting the national HIV sentinel surveillance surveys and their efforts to improve the system. We are grateful to our Chinese colleagues at NCAIDS, Drs Zunyou Wu, Ning Wang and Jiangping Sun, for their strong support for this evaluation activity. Appreciation particularly goes to Dr Lu Wang and her fellows at the Epidemiology Division of NCAIDS, including Drs Shuquan Qu, Wei Guo, Lin Ge, Dongming Li, Liyan Wang, Lan Wang, Faxin Hei, Fangfang Chen, Qianqian Qing and Zhengwei Ding, for their coordination effort and comments on the evaluation report. We would also like to thank the provincial and local C-CDC staff in Jiangxi province, Guizhou province, Shandong province and Chongqing municipality.
Members of the evaluation team were: US CDC Global AIDS Program – China office: Wen Lin, Mingshan Qi, Ling Hao; United States CDC (Atlanta): Sanny Chen; World Health Organization (China): Nicole Seguy; World Health Organization (Viet Nam): Keith Sabin; United Nations Joint Programme on HIV/AIDS (UNAIDS) (China): Zhongdan Chen.
Note: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the United States CDC. Use of trade names and commercial sources are for identification purposes only and does not imply endorsement by the Public Health Service or the United States Department of Health and Human Services.