a China Field Epidemiology Training Programme (CFETP) Beijing, China.
b Songjiang Center for Disease Control and Prevention, Shanghai, China.
c Jiangxi Provincial Center for Disease Control and Prevention, Jiangxi, China.
Correspondence to Huijian Cheng (e-mail: ejian2373@sina.com).
To cite this article:
Wang R et al. An outbreak of acute gastroenteritis associated with contaminated bottled water in a university – Jiangxi, China, 2012. Western Pacific Surveillance and Response Journal, 2012, 3(4):20–24. doi:10.5365/wpsar.2012.3.4.009
Background: On 23 May 2012, a university in Jiangxi, China reported a gastroenteritis outbreak. We investigated the outbreak to identify the agent, source and mode of transmission and to recommend control measures.
Methods: A case was defined as any person from the university with onset of diarrhoea (>3times/24h) from 1 to 31 May 2012. Active case finding was conducted by reviewing university hospital and drug-store records and interviewing students, workers and teachers. We then conducted a case-control study in which we compared food, water and environmental exposure history. Water samples were collected and tested.
Results: We identified 417 cases – an attack rate (AR) of 4.7% (417/8781) for the university. There were 416 student cases (AR = 5.7%) distributed across all 11 colleges, five of which were more heavily affected (AR range = 5.9%–14%). In the case-control study, cases had higher odds of having drunk bottled water (odds ratio [OR] = 4.1; 95% confidence interval [CI] = 1.7–9.9), and there was a dose–response relationship (X2trend = 4.6, P < 0.05). Drinking boiled bottled water was inversely associated with being a case (OR = 0.22, 95% CI = 0.07–0.71). Eating in any of the three university canteens or drinking water from the city water supply was not associated with being a case. Pathogenic Escherichia coli was isolated from two unopened bottled water specimens and from four student cases.
Conclusion: This gastroenteritis outbreak was most likely caused by contaminated bottled water. The company in question has been shut down and no further cases have been reported. Increased regulation of bottled water plants and better coordination between different investigators for future outbreaks is recommended.
In May 2012, a university in Jiangxi province, China notified the Jiangxi Provincial Center for Disease Control and Prevention (JXCDC) of a gastroenteritis outbreak with more than 70 students affected in the previous week. The university is located in the northwest of Nanchang City and comprises two teaching buildings, four laboratory buildings, 15 student dormitories, three canteens, one faculty residence and one kindergarten. The total number of students, teachers and canteen workers was 8871.
China Field Epidemiology Training Programme (CFETP) along with JXCDC investigated this outbreak to identify the agent, source and mode of transmission and to recommend control measures.
A case was defined as any person in the university with onset of diarrhoea (>3times/24h) from 1 to 31 May 2012. Active case finding was conducted by reviewing university hospital medical registration and drug-store-records and interviewing university canteen workers, students and teachers from each college. Attack rates were calculated using population numbers (teachers, students and canteen workers) in the university as the denominator. We used a structured questionnaire, which included questions on food and water exposures and other environmental factors. To determine attack rates for each of the three canteens in the university we reviewed the students’ electronic dining records as well as interviewing the students about their dining habits.
We then conducted a case-control study from 21 to 23 May and selected 106 new student cases during this period. One hundred and six students from the same dormitories as the cases were selected as controls; they were excluded if they reported any gastrointestinal symptoms. We used a more specific questionnaire that focused on drinking-water. These exposures were then compared, and analysis was conducted using SAS 9.1.3.
From 16 to 21 May, nine unopened bottled water specimens from six batches, 10 water specimens from drinking-water machines in cases’ dormitories and six water specimens from the city water supply were collected for testing. The water from the drinking machines was from the same factory that provided the bottled water. The total bacteria count and the coliform bacteria count of water specimens were tested according to the Chinese national standard examination methods for drinking-water (GB/T5750.12–2006).1
Two faecal specimens and 25 anal swabs were collected from untreated student cases from 22 to 24 May. Faecal and anal swab specimens were cultured on sorbitol-MacConkey medium for Escherichia coli and classified by serum agglutination, and tested for Escherichia coli toxin gene by polymerase chain reaction (PCR). Salmonella, Shigella and Staphylococcus bacteria, vice haemolytic vibrio, cholera, haemolytic streptococcus, liszt’s bacteria, gas single spore bacterium, pseudomonas bacteria, rotavirus, stellate virus, adenovirus, intestinal virus and goblet virus were also tested in the water, faecal and anal swab specimens.
We interviewed 8871 persons during active case finding, and 7360 of these were students. There were 417 cases of gastroenteritis in the university – a total attack rate (AR) of 4.7% (417/8781). After diarrhoea, clinical symptoms mainly included abdominal pain (64%), bloating (50%), vomiting (17%) and fever (8%). The median duration of illness was three days (range one to five days).
The onset date of the first case was 10 May with case numbers escalating from 14 May. This then levelled off from 16 to 23 May to about 50 cases each day. (Figure 1) The investigation commenced on 24 May and the bottled water was recalled later on the same day. This gastroenteritis outbreak lasted for 19 days.
There were 416 student cases (AR = 5.7% [416/7360]) with 223 males (AR = 5.2%) and 193 females (AR = 6.3%); females were more likely to be a case (relative risk [RR] = 0.82, 95% confidence interval [CI]: 0.68–0.99). The remaining case was a cook. The 416 student cases were distributed across all 11 colleges. Five of these colleges were heavily affected (AR range = 6%–14%), with the ARs of the six other colleges ranging from 2% to 5%. The ARs of the 11 colleges were statistically different (X2 = 167, P < 0.01). The AR for canteen 1 was 14% (229/1667), canteen 2 was 12% (270/2333) and canteen 3 was 11% (189/1675); there was no statistical difference between them (X2 = 5.9, P = 0.05).
The case-control study found that 92% of student cases drank bottled water compared to 73% of control-students (odds ratio [OR] = 4.1; 95% CI = 1.7–9.9). Drinking boiled water was inversely associated with being a case, and there was no difference between cases and controls that reported drinking mainly bottled mineral water (Table 1).
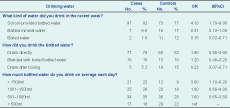
OR – odds ratio; CI – confidence interval
Among the students who reported they drank mainly bottled water in the past week, drinking bottled water directly had a higher odds ratio, while drinking bottled water after boiling had a lower odds ratio (OR = 0.22, 95% CI = 0.07–0.71). Moreover, there was a dose response relationship for student cases who drank more bottled water (from <500 ml/day to >1500 ml/day) (?2trend = 4.6, P < 0.05) (Table 1).
The total bacteria count and the coliform bacteria count of the nine unopened bottled water specimens and 10 water specimens from drinking-water machines exceeded national standards. Water specimens from the city water supply complied with the national drinking-water standard. Escherichia coli O157 and Enterotoxigenic Escherichia coli (ETEC) O55:K19 were isolated from two unopened bottled water specimens.
Enteropathogenic Escherichia coli (EPEC) O126:K71, EPEC O125:K70, EPEC O44:K74 and ETEC O15:K17 were isolated from one faecal and three anal swabs, respectively. The ETEC O15:K17 from the faecal specimen was verified as heat labile toxin positive, with all other pathogenic bacteria testing negative for the toxin.
In this university gastroenteritis outbreak investigation, the most likely source of the outbreak was contaminated bottled water. The case-control study showed that the odds of cases reporting that they mostly drank bottled water in the week before the outbreak was four times higher than the controls; there was a dose response relationship as student cases who drank more bottled water had higher ARs. The total bacteria count and the coliform bacteria count of bottled water specimens and water specimens from the drinking-water machines exceeded national standards, and the bottled water was also contaminated with pathogenic Escherichia coli. Also, after the implementation of comprehensive control measures such as recalling the contaminated bottled water, conducting safe-drinking education and rinsing dormitory drinking-water machines, the number of diarrhoea cases in the university reduced sharply.
It is unlikely that this outbreak was caused by food exposure in university canteens as the three canteens had different managers and served different food, and the student AR of each of the three canteens was not statistically different. Also, the epidemic curve suggested a continuing common source as the exposure mode; canteen food is therefore an unlikely source due to the turnover of meals at the canteens. It was also unlikely that the city water supply was the cause of the outbreak. City water is provided at student dormitories, canteens, the faculty residence and the kindergarten; there was no case from the teacher communities or the kindergarten so we assumed that the city water was not associated with the outbreak.
Until the middle of the 20th century, Escherichia coli had been regarded as a nonpathogenic bacteria to humans and part of the normal intestinal colony.2 However, some serotypes of Escherichia coli are pathogenic both to human and animals, especially infants, resulting in serious diarrhoea and sepsis. In bad environmental conditions, Escherichia coli can be dispersed with faeces. The presence of Escherichia coli in water or food indicates faecal contamination and embodies the possible existence of intestinal pathogenic bacteria. Therefore, the coliform bacteria count is generally regarded as the hygiene standard for drinking-water and food. That the coliform count was higher than the standard in the bottled water in this outbreak investigation suggests faecal contamination at some part of the production cycle of the bottled water.
In recent years, bottled water has become more popular in China because of its lower price and because it can be drunk directly.3 However, as the public health surveillance of bottled water lags behind in China, and as people will drink bottled water directly without boiling, exposure to contaminated bottled water can cause serious gastroenteritis outbreaks. Other gastroenteritis outbreaks related to Escherichia coli-contaminated bottled water have also been reported in field investigations in China.4,5
There are some limitations in this investigation. As the occurrence of this outbreak was hidden, since the symptoms of diarrhoea were light and most cases did not go to hospitals for treatment, there was a delay in the discovery and report of the outbreak. We collected only two faecal specimens, with only one heat labile toxin ETEC O15:K17 isolated. Although ETEC O15:K17 fits the clinical characteristics of the cases and the epidemiology of the outbreak, we cannot definitively state that ETEC O15:K17 was the causative agent. For future outbreaks, we recommend that investigators increase the proportion of faecal specimens collected.
The large decline in cases after our investigation and the recall may be due to the fact that at this stage we conducted active case finding through university hospital doctors only, not by interviewing each students as we did during the investigation. Due to the light clinical symptoms, some student cases may not go to hospitals despite knowing about the outbreak. This probably was the reason why case numbers decreased quickly after 24 May. We were also unable to acquire incidence information from other schools in which bottled water was supplied by the same water company. This was because the water company manager refused to talk with our investigators and we were unable to inspect the company premises. We were therefore also unable to ascertain possible pollution sources and steps, or determine the source of the contamination.
As a result of this outbreak, we recommended that the water company stop producing bottled water and identify the contamination source. On 3 June, the water company was shut down by the Nanchang Bureau of Quality and Technical Supervision. To prevent future outbreaks, we also suggested that the long-term regulatory oversight and surveillance of bottled water be enhanced to ensure the security of drinking-water. During future outbreaks, we also recommend that departments such as the Centre for Disease Control and Prevention, Food and Drug Administration, Bureau of Health Supervision and Bureau of Quality and Technical Supervision share results and findings and conduct investigations collaboratively.
None declared.
None.