a Head, Department of Epidemiology, Ha Noi School of Public Health, Ha Noi, Viet Nam
Correspondece to Lan Thi Hoang Vu (e-mail:vhl@hsph.edu.vn).
To cite this article:
Lan TV. High-risk and multiple human papillomavirus infections among married women in Can Tho, Viet Nam. Western Pacific Surveillance and Response Journal, 2012, 3(3):57-62. doi:10.5365/wpsar.2012.3.1.007
Introduction: The two currently licensed human papillomavirus (HPV) vaccines are highly efficacious in preventing cervical pre-cancers related to HPV 6, 11, 16 and 18. Before implementing a large-scale HPV vaccine campaign in Viet Nam, information about the prevalence of infection with the HPV vaccine types is required. This study was done in Can Tho, the province with the highest prevalence of cervical cancer in the south of Viet Nam, to explore the distribution of other high-risk types of HPV among married women in this province.
Method: The study employed a cross-sectional design with multistage sampling. A total of 1000 participants were randomly selected, interviewed and given gynaecological examinations. HPV infection status and HPV genotyping test were completed for all participants.
Results: A broad spectrum of HPV types was reported in this study. The prevalence of cases infected with HPV 16 and/or 18 was 7%; the prevalence of cases infected with other high-risk HPV types was 6%. The highest prevalence for single and multiple infections, as well as for high-risk infections, was reported for the youngest age group (less than 30 years).
Discussion: While it is relevant to implement an HPV vaccine campaign in Viet Nam due to the high prevalence of infection with HPV 16 and/or 18, it is important to note that one can be infected with multiple types of HPV. Vaccination does not protect against all types of high-risk HPV. Future vaccine campaigns should openly disclose this information to women receiving vaccines.
Cancer of the cervix is the second most common cancer in women worldwide with about 500 000 new cases and 250 000 deaths each year.1 Almost 80% of cases occur in low-income countries where cervical cancer is the most common cancer in women. Previous studies attributed the large decline of cervical cancer incidence in developed countries to their screening programmes and suggested that the high rate of cervical cancer mortality and morbidity in developing countries was due to ineffective or no screening programmes.2 In 2010, Viet Nam had a total of 5644 cervical cancer cases (prevalence of 13.6 per 100 000 women).3
However, the prevalence rate in the south of Viet Nam is much higher, at about 26 per 100 000 women.3,4 The steadily increasing rate of this cancer in some provinces in the south has been observed in recent years. For instance, the crude rate of cervical cancer in Can Tho was only 15.7 per 100 000 in 2000 but increased to 25.7 per 100 000 in 2009.3
Studies have shown that infection with high-risk human papillomavirus (HPV) can lead to cervical cancer.5,6 Specifically, high-risk HPV types are detected in 99% of cervical cancers, and worldwide approximately 70% of cervical cancers are due to HPV types 16 and 18.7–10 In developed countries such as the United States of America, vaccines against HPV were recommended for routine use in females aged 11 to 12 years.11 In Viet Nam, HPV vaccines have been offered since 2006. These vaccines are expensive for developing countries (US$ 80 per dose with three doses required). These vaccines, however, prevent only four HPV types, two high-risk types (HPV 16, 18) and two low-risk types (HPV 6, 11).11,12
Before implementing a large-scale HPV vaccine campaign in the south of Viet Nam, updated data on the prevalence and distribution of the vaccine types of HPV among women is required. During 2010 and 2011, a large-scale study was done in five provinces (Ha Noi, Ho Chi Minh City, Hue, Thai Nguyen and Can Tho) to explore the prevalence of HPV infection and its risk factors.13–15 The prevalence of cervical HPV infection ranged from 6.1% in Ha Noi to 10.2% in Can Tho. Most of the positive cases were infected with high-risk HPV, especially in Ha Noi and Can Tho where more than 90% positive cases were high-risk HPV. Furthermore, in Can Tho, more than 60% of women were infected with multiple HPV types.15
This study provides additional data to explore the distribution of HPV among married women in Can Tho in order to provide more detailed information for the cervical cancer prevention programme in this province.
Can Tho is located on the south bank of the Hau River, a major branch of the Mekong River. It is 169 km from Ho Chí Minh City, Viet Nam’s largest city. Can Tho is the fourth largest city in Viet Nam and the biggest city in the Mekong Delta with an estimated population of 1 187 089. The majority of the population is living in urban areas (66%). The city is divided into nine districts and 85 communes. After 120 years of development, the city now is the delta’s most important centre of economics, culture, science and technology.
This study applied a cross-sectional design and multistage sampling as described elsewhere.13–15 The estimated sample size was 1050 women using a formula for sample size for a proportion estimate with relative precision with the following parameters: anticipated prevalence of HPV as 10%, relative precision of 0.25, design effect of 1.6 and estimated non-respondent rate of 10%. In the first stage, 21 communes were randomly selected from 85 communes in Can Tho. In the second stage, in each commune, 50 married women aged 18–65 were randomly selected from the list provided by the local women’s union (this list contains the names of women currently living in the commune). Following an explanation about the objectives of the study, a written consent form for participation in the study was completed. The response rate was high (95.2%) and the final sample size was 1000 women. The main reason women declined to participate was that they were uncomfortable with pelvic examination.
Information and specimen collection used the following steps. First, a personal interview was done to collect information on socio-demographic variables, obstetric/gynaecologic history and sexual lifestyle. After the interview, each participant was scheduled for a pelvic examination carried out by a gynaecologist. Samples of exfoliated cells from the ectocervix were collected with two wooden Ayre spatulas and were sent to the laboratory of the Viet Nam National Institute of Dermatology for HPV testing on the same day as the sample collections. The HPV genotyping protocol was described elsewhere.13 The protocol was reviewed and cleared by the Ha Noi School of Public Health Institutional Review Board (Ethical Approval Number 013/2010/YTCC-HD3).
High-risk HPV types are those that can cause cancer and include HPV 16, 18, 31, 33, 35, 39, 45, 51, 52, 53, 56, 58, 59, 66, 68 and 82. The low-risk group includes HPV 6, 11, 42, 43, 61, 70, 71 and 81. The current vaccines can prevent only high-risk types 16 and 18, and low-risk types 6 and 11. Infection with HPV 16/18 in this study refers to cases infected with either HPV 16 or HPV 18 or with both of these types.
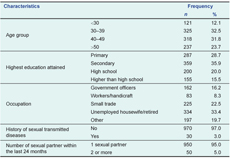
Most women who participated in this study were aged from 30 to 49 years (64%). A total of 30 women (3%) reported a history of having been diagnosed with sexual transmitted diseases, with 5% reporting having more than two sexual partners within the last 24 months (Table 1).
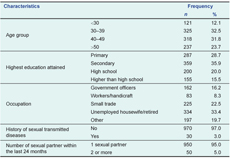
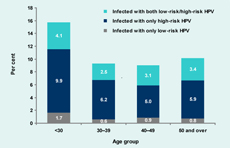
Most infected cases in this study had infections with multiple types of HPV, and this was shown for each age group (Figure 1). The prevalence of multiple HPV infection was highest among the youngest group at 7.4%. About 60% of the cases with multiple HPV infection were infected with more than two types of HPV; some cases were even infected with five or six different HPV types.
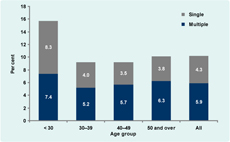
In total, 73% of the positive cases were infected with HPV type 16/18; however, more than half of these cases were also positive with other high-risk types. More importantly, 19% of positive cases were not infected with HPV16/18 but with other high-risk types (Figure 2). Overall, the prevalence of cases infected with HPV 16/18 was 7% and the prevalence of cases infected with other high-risk HPV types (including those infected with HPV 16/18 in addition to other high-risk infection types) was 6% (total 58 women).
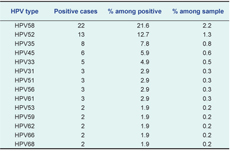
In addition to HPV 16 and 18, there were 14 other high-risk HPV types identified in this study (Table 2). HPV 58 and HPV 52 were the most common of these high-risk types found in Can Tho, accounting for 22% and 13% of the positive cases, respectively.
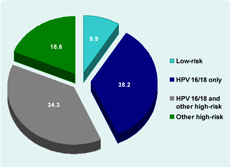
Analysis by age group showed that (1) in all age groups, most cases were infected with high-risk HPV, which can lead to cancer; (2) the overall prevalence of HPV infection (i.e. including both low-risk/high-risk) was highest among the youngest group (i.e. less than 30-years-old); and (3) the prevalence of infection with high-risk HPV was also highest among the youngest group (Figure 3).
A broad spectrum of HPV types was reported in this study. The prevalence of cases infected with HPV 16/18 was 7% and the prevalence of cases infected with other high-risk HPV types was 6%. The most common types of HPV infection were HPV 16 and 18, similar to previous studies in Viet Nam and other countries.16–18 HPV 58 was also found to be a common type among women in Can Tho, as reported in China, Thailand and The Philippines.6 The higher prevalence reported for Can Tho is consistent with the higher rate of cervical cancer in the southern compared to the northern provinces of Viet Nam. Previous studies had reported that the higher rate of cervical cancer in southern Viet Nam could be attributed to the ground combat militarization of South Viet Nam during the period 1955–1975.19
Similar to a previous study,14 the prevalence of overall HPV infection as well as the prevalence of high-risk HPV infection was highest among the youngest group (aged less than 30-years-old). This result demonstrates the increasing trend of HPV infection among the younger generation in Viet Nam as well as the need for effective cervical cancer programmes. A recent study suggested that the best control programme for cervical cancer in Viet Nam is to offer HPV vaccine to young girls and screening to older women. An 70% vaccination and screening coverage rate would reduce the lifetime risk of cancer by 20.4% to 76.1%.20
Some health organizations in Viet Nam are considering two types of HPV vaccines licensed by the Food and Drug Administration (i.e. Cervarix made by GlaxoSmithKline and Gardasil made by Merck).12 Cervarix protects against only HPV types 16 and 18, while Gardasil also protects against HPV types 6 and 11. It is important to note that one woman may be infected with multiple types of HPV at once. While 73% of the positive cases were infected with HPV 16/18, more than half of these were also infected with other high-risk HPV types that may also lead to cervical cancer and which cannot be prevented by currently available vaccines. Although it is relevant to implement an HPV vaccine campaign in Viet Nam due to the high prevalence of infection with HPV 16/18 in Can Tho, it is also important to inform the women who receive the vaccines that they are not protected against all high-risk HPV types and that they still need cervical cancer screening.
In developed countries, routine Pap smear and HPV tests are recommended for screening for cervical cancer. The Pap test is a method of examining cells from the cervix and is suggested every one to two years for most women aged 21 to 29 and every two to three years for most women aged 30 or older. For women aged 30 or over, HPV tests can be done in addition to Pap smear tests.21 As with other developing countries, Viet Nam has not yet established a national policy and guidelines on cervical cancer screening.
Strict protocols to avoid biases were followed in this study: women were randomly chosen, all clinical examination and specimen collections were done by qualified gynaecologists and all samples were examined by a nationally qualified laboratory. The detection of HPV positivity using real-time polymerase chain reaction methods and the genotyping of HPV type using reverse dot blot method in this study also provided more precise results compared to the Hybrid Capture Tube Method applied in previous studies.17 However, it is important to note that this study covered only married women aged 18–65 so the results did not cover a subgroup of the population already sexually active but not yet married. This is a limitation of the study, but under the cultural and ethical norms of Viet Nam, it is very difficult to invite unmarried women to participate in a study with pelvic examinations. Women in Can Tho are also getting married at a later age, which further restricted the involvement of younger women in the study. Since the prevalence of HPV was higher in the younger age group in this study, and this group was under-represented due to the sampling frame, the actual prevalence in Can Tho might be higher than reported.
Since the findings of this study came from one urbanized province in the south of Viet Nam, caution must be taken in generalizing these findings to the entire Viet Nam population, especially to those in rural areas. In conclusion, a high prevalence of HPV infection, especially high-risk types, was observed in this study and this was higher for younger married women. As HPV infection has a high correlation with cervical cancer, this study emphasizes the need for both primary prevention of cervical cancer with HPV vaccines as well as secondary prevention with screening. Policy-makers in Viet Nam should consider making HPV vaccines and screening for cervical cancer routine practices.
None declared.
None.