
a Public Health Unit, Sydney South West Area Health Service, Sydney, Australia.
b Foodborne Illness Investigation Unit, New South Wales Food Authority, Sydney, Australia.
Correspondences to Sophie Norton (e-mail: Sophie.Norton@sswahs.nsw.gov.au).
To cite this article:
Norton S et al. A large point-source outbreak of Salmonella Typhimurium linked to chicken, pork and salad rolls from a Vietnamese bakery in Sydney. Western Pacific Surveillance and Response Journal, 2012, 3(2):16-23. doi:10.5365/wpsar.2012.3.1.001
Introduction: In January 2011, Sydney South West Public Health Unit was notified of a large number of people presenting with gastroenteritis over two days at a local hospital emergency department (ED).
Methods: Case-finding was conducted through hospital EDs and general practitioners, which resulted in the notification of 154 possible cases, from which 83 outbreak cases were identified. Fifty-eight cases were interviewed about demographics, symptom profile and food histories. Stool samples were collected and submitted for analysis. An inspection was conducted at a Vietnamese bakery and food samples were collected and submitted for analysis. Further case ascertainment occurred to ensure control measures were successful.
Results: Of the 58 interviewed cases, the symptom profile included diarrhoea (100%), fever (79.3%) and vomiting (89.7%). Salmonella Typhimurium multiple-locus-variable number tandem repeats analysis (MLVA) type 3-10-8-9-523 was identified in 95.9% (47/49) of stool samples. Cases reported consuming chicken, pork or salad rolls from a single Vietnamese bakery. Environmental swabs detected widespread contamination with Salmonella at the premises.
Discussion: This was a large point-source outbreak associated with the consumption of Vietnamese-style pork, chicken and salad rolls. These foods have been responsible for significant outbreaks in the past. The typical ingredients of raw egg butter or mayonnaise and pate are often implicated, as are the food-handling practices in food outlets. This indicates the need for education in better food-handling practices, including the benefits of using safer products. Ongoing surveillance will monitor the success of new food regulations introduced in New South Wales during 2011 for improving food-handling practices and reducing foodborne illness.
In Australia, it is estimated that there are 5.4 million cases of gastroenteritis caused by contaminated food each year, accounting for approximately one third of all gastroenteritis cases in the country. Consequently there are 1.2 million visits to doctors, 18 000 hospital admissions and approximately 120 deaths annually due to foodborne illness.1 Various types of Salmonella are commonly identified as the etiological agent and Salmonella Typhimurium (STM) is the most commonly notified serovar in Australia.2
On 4 January 2011, a hospital emergency department (ED) in Sydney, Australia notified the Sydney South West Public Health Unit (SSWPHU) of an increased number of gastroenteritis presentations during the previous evening. On the same afternoon three cases were interviewed; however, no common exposures were identified.
The next day, the hospital notified SSWPHU of additional gastroenteritis cases presenting overnight, with all patients reporting consumption of pork or chicken rolls from a bakery in the area. An outbreak investigation was initiated incorporating epidemiological, environmental and laboratory elements. This paper describes the public health investigation and response to a foodborne outbreak caused by STM from a commercial food outlet.
Case-finding was conducted by requesting daily reports from five EDs closest to the bakery premises. General Practitioners (GP) in the local area and other Public Health Units in New South Wales (NSW) were alerted to the outbreak and asked to report possible cases. EDs and GPs were also asked to take stool samples from possible cases. A possible case was defined as: an individual with diarrhoea and either vomiting or fever, with an illness onset after 1 January 2011 and who attended a hospital ED or a GP practice.
To confirm that food from the bakery was the only common exposure, detailed food histories for the three days preceding illness onset were obtained for the first 26 cases notified to SSWPHU. Other possible cases were interviewed using a shorter standardized questionnaire to confirm exposure, onset date, symptoms, date of exposure and details of foods consumed from the bakery. Where a person was unable to be contacted directly, a cases linkage to the bakery was verified by clinician documentation in electronic hospital notes, direct discussion with the treating clinician or a relative.
Subsequently, after an association with food consumed from the bakery was established, a bakery-linked case was defined as an individual with diarrhoea and/or vomiting or fever with illness onset after 1 January 2011 and who ate food prepared at the bakery between 30 December 2010 and 5 January 2011.
Bakery staff were also interviewed using the standardized questionnaire to identify illness and exposure details.
Data were entered in Microsoft Excel 2007 and analysed using Statistical Analysis Software (SAS) System version 9.2.
The NSW Food Authority, the regulatory body responsible for food safety in NSW, was notified of the outbreak on the orning of 5 January 2011. An inspection of the suspect premises was conducted on the afternoon of 5 January 2011, by which time SSWPHU had conducted approximately 10 of 26 hypothesis-generating long interviews, all identifying a Vietnamese bakery at a particular street location where pork/chicken/salad rolls had been purchased in the 48 hours before illness onset.
Food-handling and cleaning practices were reviewed by the NSW Food Authority. Environmental swabs and food samples were collected from the bakery for microbial testing. Food samples included chicken, pork, ham, egg butter, mayonnaise, pate and a variety of other foods stored in the chilled food display cabinet. A trace-back of suspect foods served at the premises was initiated.
Faecal specimens were cultured at laboratories throughout Sydney. Clinical Salmonella isolates were sent to the Centre for Infectious Disease and Microbiology Laboratory Service (CIDMLS) in Sydney for typing. Food and environmental samples were tested by the Division of Analytical Laboratories. Multiple-locus-variable number tandem repeats analysis (MLVA)3,4 was performed on the clinical, food and environmental isolates by CIDMLS. Food and environmental specimens were phage typed at the Institute of Medical and Veterinary Science in Adelaide, South Australia. All results were then collated by SSWPHU. Phage typing is not routinely carried out on clinical specimens in NSW.
All Salmonella isolates within NSW are referred to CIDMLS for serotyping and MLVA typing if appropriate. STM MLVA data from the outbreak period were obtained from NSW Ministry of Health to assess whether there were other cases of the outbreak strain occurring at this time. Data with an MLVA type consistent with the investigation were compared with background rates of the same type. No extra interviews were conducted as there was a delay in reporting of MLVA data and extra interviews would not have contributed to control efforts at that point.
The SSWPHU was notified of 154 possible cases by EDs and GPs. Of these, 83 cases were identified as being linked to the bakery. Sixty-two cases were reported by EDs and GPs but were not interviewed and no information was available on place of exposure and foods consumed. Nine possible cases were interviewed and subsequently excluded. Fifty-eight of the 83 bakery-linked cases were interviewed directly, while the remaining 25 were confirmed through documentation by the clinician in electronic hospital notes accessible to SSWPHU or through discussions with the treating clinician or a relative (Figure 1).

Of the first 26 cases notified to SSWPHU, 21 (81%) had consumed food from a single Vietnamese bakery in the three days before onset of illness.
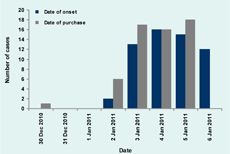
The median age of interviewed bakery-linked cases was 27.5 years (range, 1 to 75 years) and most cases were female (Table 1). The peak of the outbreak occurred between 3 and 5 January 2011, with 86% (50/58) of cases reporting disease onset on these three dates (Figure 2). The median incubation period reported was one day (ranging from less than one day to three days) with 40% (23/58) of cases reporting an incubation period of less than one day. Demographic and clinical characteristics of interviewed bakery-linked cases are contained in Table 1.
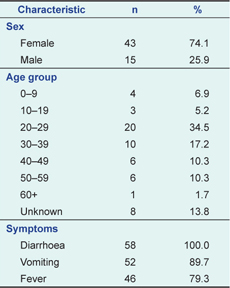
Of the 83 known bakery-linked cases, 64 (77%) sought medical attention: six (7%) cases visited a GP, 38 (46%) cases were reviewed in an ED and 20 (24%) cases were admitted to hospital.
All but one case purchased food from the bakery over a four-day period (2 to 5 January 2011). This case reported purchasing food on 30 December 2010 and became unwell on 2 January 2011, but no stool specimen was taken. No further cases were identified after the NSW Food Authority inspection on the afternoon of 5 January 2011 (Figure 2).
All 58 interviewed cases reported that they ate a roll of some type from the bakery before illness onset. Information regarding individual roll ingredients consumed by these 58 cases was collected and results are outlined in Table 2.
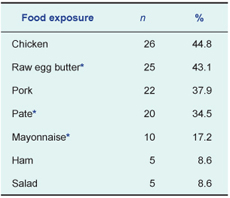
* 18 cases replied “unknown” to these food exposures
Only one staff member from the bakery reported becoming unwell during the outbreak, with an onset date of 5 January 2011. This food handler reported eating a salad roll with mayonnaise from the bakery on 4 January and a salad roll with raw egg butter on 5 January before becoming unwell. All other staff stated that they consumed food from the bakery but did not become unwell.
A total of 49 stool specimens were obtained from the bakery-linked cases. Salmonella Typhimurium MLVA type 3-10-8-9-523 was identified in 47 samples. Two cases’ specimens were negative for bacterial pathogens.
MLVA results from CIDMLS identified 89 stool samples from residents in south-western Sydney between 4 and 24 January 2011 where STM MLVA 3-10-8-9-523 was identified. Seventy-three (82%) of the samples were collected between 4 and 9 January 2011. The number of positive samples peaked on 6 January 2011, at 24 samples. Sydney West area (the neighbouring area health service that is geographically closest to the premises) saw a simultaneous increase in the same MLVA type with 14 positive stool specimens in this time period. Excluding the 47 known bakery-linked cases from the total of 105 cases in the two health areas with the same MLVA type, an additional 56 people may have been affected by this outbreak. NSW data from the same period in 2010 identified only 12 stool samples positive for STM MLVA 3-10-8-9-523.
The bakery was located within a busy shopping centre in Sydney, NSW. The NSW Food Authority inspection of the premises on 5 January 2011 revealed that there were multiple breaches of food safety standards of the Australia New Zealand Food Standards Code (Table 3).5
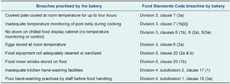
Raw egg butter was made approximately every three days by the premises. The raw egg butter batch made on 2 January 2011 was mixed with the new batch made on 5 January 2011. Raw egg butter is produced by hand by shifting egg contents back and forth between half shells to separate yolks, which are then mixed with vegetable oil and salt using metal whisks. The egg butter was not subject to a processing step such as pasteurization, adequate heating or acidifying the product.
The chicken liver pate was prepared on 2 January 2011. The same batch of each of the following ingredients was served from 2 to 5 January 2011:the pork belly which purchased and cooked on 23 December 2010, the white ham purchased on 30 December 2010 and the prager ham purchased on 23 December 2010. The chicken served to customers in the same time period was purchased and cooked on 31 December 2010, 3 January 2011 or 5 January 2011.
The bakery owner voluntarily removed and disposed of all roll fillings from the chilled food cabinet and all prepared sandwich ingredients. The bakery was asked to cease production of raw egg butter and pate until the NSW Food Authority had finalized their investigation.
On 10 January the NSW Food Authority served a prohibition order to the premises based on food sample and swab results that confirmed widespread Salmonella contamination in the store. The order closed the business until the following conditions were met: all equipment cleaned and sanitized, fixtures and fittings verified free from Salmonella by the NSW Food Authority and food handlers demonstrating adequate skills and knowledge in food safety and hygiene. The business agreed to permanently cease production of raw egg butter in accordance with the NSW Food Authority’s recommendation.
Sixty-two per cent (13/21) of the food samples were positive for STM phage type 44, MLVA type 3-10-8-9-523. These included the raw egg butter, chicken liver pate, chicken, pork and various salad ingredients. The mayonnaise was a commercial brand that was used before its expiration date. Only cooked chicken and pork were available for sampling at the time of inspection. Forty-five per cent (5/11) of the environmental swabs were also positive for STM phage type 44, MLVA type 3-10-8-9-523.
Eleven eggs left over from the batch used to produce the raw egg butter made on 2 January and 5 January 2011 were submitted for testing. No Salmonella or other organisms were isolated. The eggs used by the bakery during the outbreak were purchased on 1 January 2011 from a growers’ market in Sydney that was not the usual supplier. The egg supplier to the market stall sourced the eggs from 10 farms in NSW and occasionally from a farm in Victoria. The NSW Food Authority was unable to trace the farm of origin of the eggs used by the bakery during the outbreak due to missing labels on the egg cartons.
This was a large point-source outbreak of Salmonella Typhimurium MLVA 3-10-8-9-523 in which the majority of identified cases (77%) sought medical attention. The outbreak was probably larger than demonstrated by this investigation as indicated by the retrospective MLVA data provided by NSW Ministry of Health, which showed a clear increase at the time of the outbreak in this MLVA type compared to the usual background rate.
A major concern demonstrated by this outbreak was a clear lack of knowledge of safe food handling practices. Various forms of temperature abuse were involved in storage and display and also production of foods, such as inadequate monitoring of temperatures during cooking and inadequate cooling of food items after cooking. The business used the undesirable practices of producing raw egg butter with no pathogen control step6 and mixing ready-to-eat foods with existing batches. Several mechanisms for cross-contamination were also evidenced: the type of Salmonella responsible for the outbreak was isolated from 62% of the samples of food sold on the premises and from 45% of environmental swabs taken from utensils and surfaces used for food processing and from objects and surfaces not directly involved in food preparation.
This investigation was unable to identify the food source that introduced Salmonella onto the premises. Eggs, chicken, pork, ham and salad items have all previously been implicated in foodborne outbreaks.7–12 In this outbreak, all of these food items grew the same type of Salmonella that was identified as the cause of clinical illness, potentially implicating any of these items as the original source of Salmonella.
Nevertheless, eggs were considered the most likely potential source as the eggs used to make the raw egg butter were not bought from the usual supplier; they were stored inadequately then served raw in the form of raw egg butter; and there was no pathogen control step. Also, during the raw egg butter production, the practice of moving the contents of the egg back and forth between the two shell halves to separate the yolk allowed a route for the outer shell to potentially contaminate the contents.
Foods commonly known to contain raw egg have been identified as the cause of large point-source outbreaks, especially in commercial food outlets.2,13 Salmonella Typhimurium phage type 44 has previously been associated with consumption of raw eggs or prepared dishes containing raw eggs.14 OzFoodNet, an Australian national network set up to improve foodborne disease surveillance, management and prevention,15 reported at least 40 Salmonella outbreaks across Australia between 2009 and 2010,13,16–21 in which ready-to-eat foods containing raw egg were identified as the probable vehicle.
Pork and chicken have also been implicated as a vector of Salmonella, including outbreaks specifically implicating Vietnamese pork rolls.13,16–21 This evidence, combined with inadequate temperature checking of the pork belly during cooking and the prolonged cooling time of the chicken liver pate, suggests pork or chicken could also be the suspect food source in this outbreak. However, due to lack of epidemiological evidence pinpointing a particular food item, the fact that no STM 44 was isolated from any of the eggs tested and the inability to trace back a source farm for the eggs, confirmation of eggs or any other food as the pathogen vector in this outbreak was not successful.
Multiple factors have often contributed to large Salmonella outbreaks. These include issues related to storage and refrigeration, substandard labelling of preparation dates, mixing old with new batches of foods, using broken shells to separate egg yolk and the use of second grade eggs.14,22–25 Often there are also issues with general hygiene and cleaning practices leading to cross-contamination.15,23,26 This all suggests that food safety regulations should remain focused on these aspects of control.
Strategies to minimize the risk of Salmonella transmission to the public are taken at every level–from industry involved in food production to food services and consumers.16 The egg production industry has quality assurance standards such as egg labelling, food safety, animal health and welfare, biosecurity and environmental management.27 In June 2010 a new regulation was introduced in NSW requiring egg producers to implement a food safety programme. Voluntary industry measures coupled with government mandated measures mitigate the risk of Salmonella reaching the food services industry but will not always prevent this from occurring.23
To address issues surrounding food handling, the NSW government has introduced new regulations under the Food Amendment (Food Safety Supervisors) Bill 2009. This initiative, introduced in October 2010, required food businesses such as hospitality and food retailers to have at least one trained Food Safety Supervisor (FSS) appointed in the business by 1 October 2011. Training occurs through registered accredited training organizations. It remains mandatory for all food handlers to have general knowledge and skills appropriate to their role, as outlined in the Food Standards Code.28–30
It was not possible to present an association between foods consumed and illness because we did not recruit controls. We felt it would have been difficult to find a comparison group and unnecessary given that we already had strong evidence pointing to the bakery. This investigation was only capable of capturing the more severe cases and therefore does not reflect the true magnitude of the outbreak. Many interviewed cases did not supply more detailed information regarding condiments contained on their rolls because they did not know or could not remember. Finally, an analytic study would have been difficult to justify in these circumstances because the premises was the point of control, and control was achieved through closure without having to identify the exact source.
Two of the seven food handlers were unable to be interviewed. They were both family members of the business owner and only anecdotal information on the absence of illness was able to be obtained. Also, a detailed history of foods eaten in the specified time period was not obtained from these two food handlers.
This large outbreak was associated with a single Vietnamese bakery and significantly affected the health of individuals and put stress on the health system. Foodborne disease is a great public health concern as the effects of outbreaks cause considerable morbidity and consume public health effort and resources.31 These outbreaks are essentially avoidable. Poor understanding of food handling practices, leading to extensive cross-contamination throughout the bakery, played a major role in this outbreak. This issue has contributed to other large point-source outbreaks in the past. The introduction of new regulations such as the FSS Programme could contribute, through improved hygiene education, to minimize the extent of contamination and therefore the size and severity of outbreaks in many instances in the future. The role of NSW Ministry of Health and the NSW Food Authority in reacting promptly to food complaints and laboratory information that indicate a possible common exposure to Salmonella that continue to be crucial in future regulatory changes.
None declared.
None.