a Taro National Health Insurance Clinic, Miyako City, Iwate Prefecture, Japan (e-mail: qurodaj98@yahoo.co.jp.)
To cite this article:
Kuroda H. Health care response to the tsunami in Taro District, Miyako City, Iwate Prefecture. Western Pacific Surveillance and Response Journal, 2011, 2(4):17-23. doi:10.5365/wpsar.2011.2.4.001
Problem: In the Taro District (population: 4434), the great tsunami of 11 March 2011 destroyed the central region including the clinic, the sole medical facility (one physician, 13 nurses and other staff) in the district, and many citizens were forced to live in evacuation centres.
Context: The Taro District experienced massive damage during the tsunamis of 1896 and 1933. Since then countermeasures to tsunamis have been implemented. The great tsunami on 11 March 2011 caused catastrophic damage to the low-lying areas where approximately 2500 people lived; 1609 buildings were completely destroyed, and approximately 200 people died or were missing across the district.
Action: The Taro National Health Insurance Clinic, the sole medical facility in the Taro District, was required to play a central role in a variety of activities to care for residents in severely affected areas. First of all, evacuees needed to move to neighbouring hospitals or safer evacuation centres because lifeline services were cut off to the first evacuation centre. Then, the clinic staff worked in a temporary clinic; they visited the evacuation centres to assess the public health and medical situation, cared for wounded residents, managed infection control and encouraged a normal lifestyle where possible. Additional medical, pharmaceutical and logistical support was received from outside the district.
Outcome: There was no noticeably severe damage to health, although there was manifestation of and deterioration in lifestyle-related diseases (e.g. diabetes, hypertension, obesity). Health care activities gradually returned to their pre-disaster levels. At the end of July 2011, the evacuation centres closed, and all evacuees moved to temporary accommodations.
Discussion: Isolated rural health practitioners were required to be involved in a wide variety of activities related to the disaster in addition to their routine work: e.g. preventive health (public health and safety activities), routine medical care, acute medical care, psychological care, post-mortems and recovery of medical facilities. Although the whole health care system returned to near-normal six months after the disaster, it is important to plan how to develop more resilient medical systems to respond to disasters, especially in rural areas. This article describes my experience and lessons learnt in responding to this disaster.
Compared to the rest of Japan, the coastal region of Iwate Prefecture has a shortage of medical services.1 The Taro District (Figure 1), Miyako City, Iwate Prefecture is no exception. The sole medical facility in the district was for some time the Taro Municipal Hospital (established in 1948); the district hospital was restructured into a municipal clinic with inpatient facilities (19 beds) in 2010. Since 2007, I have been the only doctor in the district. In addition, there are 13 nurses, one clinical laboratory technician and one radiation technician in the clinic. Before the earthquake, there was a daily average of 57.5 outpatients and 9.6 inpatients; home visits were made to approximately 30 people per month (as of FY 2009).2
* Taro District, Miyako City is located near the centre of the coastal region of Iwate Prefecture, facing the Pacific Ocean. Shimonoseki City, the most western of Honsyu island, dispatched health care workers to Miyako City, the most eastern city. Ryukyu National Hospital stands on Okinawa.
As the only doctor, I was responsible for (1) primary/internal medical care for outpatients/inpatients; (2) public health activities; (3) school-based medical care at day care centres, elementary schools, junior high schools, high schools; (4) visiting medical care at elder homes; (5) various immunizations; (6) health checkups and (7) health seminars.
The tsunami that struck on 11 March 2011 destroyed much of the central region including the clinic (Figure 2). Many local citizens were forced to move to the evacuation zones due to the extent of the destruction in the affected area (Figure 3).

* A giant wave overcame the 10-metre high embankment and destroyed the central region including the clinic on 11 March 2011. Our clinic is seen in the left of this photo (marked with an arrow), which was taken from the 3rd floor of a building overlooking the north-west direction. Reproduced with permissions from Mr M Hatakeyama.

* By 12 November 2011, almost all destroyed buildings and rubble have been removed. Our clinic is seen the middle of this photo (marked with an arrow), which was taken by the author from a10-metre high countermeasure embankment.
In the context of a shortage of medical services and the destruction of the only medical facility, this paper describes the lessons learnt on the evacuation, maintenance of people’s health, continuation of medical activities and support received from inside and outside the district.
The Taro District, Miyako City, Iwate Prefecture encompasses an area of 101 km2 with a population of 4434 people (as of 1 March 2011).3 It is located near the centre of the coastal region of the Iwate Prefecture; its main industries are fishing and tourism, and it is characterized by a declining population, falling birth rates and an aging population.3
The Taro District experienced massive damage in the tsunami of 1896 (wave height: 15 m; fatalities: 1859 people; survivors: 36 people) and that of 1933 (wave height: 10 m; fatalities: 911 people; survivors: 1828 people).4,5 Countermeasures against tsunamis have since been implemented including setting up of an embankment with a total length of 2.4 km and a height of 10 m (Figure 3), flood protection forests, remote control floodgates, deployment of illuminating lights using solar panels, deployment of public address radio networks for disaster control to each household, tsunami observation systems, annual tsunami evacuation drills and educational activities undertaken by people who had experienced the tsunami of 1933.4,5 In March 2003, a municipal proclamation on tsunami disaster control was announced by the authorities.
On 11 March 2011, the great tsunami, following a magnitude 9.0 earthquake, struck the Pacific coast of eastern Japan. Approximately 20 000 people were dead or missing, and about 120 000 buildings completely destroyed.6 Approximately 330 000 people remained refugees as of November 2011.7 In the Taro District, the waves reached over 30 m in height.8 Taro was one of the regions with the highest waves and the most damage.
The 11 March 2011 tsunami and earthquake overwhelmed the engineering countermeasures. Most of the low-lying areas (approximately 2500 residents) were affected by the tsunami and 1609 buildings were completely destroyed. Approximately 200 people were dead or missing across the Taro District.
The Taro National Health Insurance Clinic was completely destroyed by the tsunami, but all five inpatients and staff in the clinic were successfully evacuated to a hill 500 m from the clinic. Within a day, we set up a temporary outpatient clinic in the General Affairs Office, which is located in a less affected area. We set up inpatient care functions in a meeting room of the nursing care facility on the following day.
In the centre of the town, which was severely damaged, approximately 800 residents evacuated to the three temporary evacuation facilities. The evacuation facilities were surrounded by rubble, tsunami seawater and a fire on the night of 11 March. I started triage on the morning of 12 March to identify the evacuees with health problems who required nursing care. Almost all the vulnerable people (approximately 20 in number) with health problems were transported to nearby hospitals and nursing care facilities on 12 March. In addition, I undertook post-mortems in the district at the request of the local police force.
The majority of evacuees did not have their regular prescriptions with them in the evacuation centres and needed them as quickly as possible. However, the clinic, which was the only pharmacy in the district, was destroyed by the tsunami. Evacuees including clinic staff were left with no lines of communication.
On 12 March, the nurses at the clinic went through the wreckage of the clinic and salvaged important medical products (antihypertensives, aspirin, acid suppressions, antimicrobials, antipyretic-analgesics, anti-anxiety agents and laxatives). Since the printed medical records had all been lost in the disaster, filling prescriptions for regular medicines was done by my memory following requests from patients. A computer server that stored prescription details at the clinic was later recovered.
On 15 March, the clinic was moved to a location with better access for delivery of miscellaneous medicines. From 25 March, pharmacists from outside the district helped to manage medicines. On 4 July, external prescription dispensing began at a pharmacy.
Medical and nursing staff were concerned that infection9 and thromboembolism10 would become problems for the evacuees and implemented prevention measures such as hand–washing, gargling, cleaning, periodic ventilation, encouragement of “radio gymnastic exercises” (a common national exercise in Japan) and drinking ample water.
Neighbourhood resident groups, who were not affected by tsunami, volunteered to serve rice balls beginning on the first day of the disaster. Safe drinking-water was available, including stocked bottled water, at the evacuation centres.
My clinic staff visited several evacuation centres to assess the situation, respond to suffering people and manage contagious diseases. As insomnia, constipation and acute upper respiratory tract inflammations had become significant issues among the evacuees, staff at the evacuation centres prescribed anti-anxiety agents, laxatives and cold remedies.
On 1 April, 800 people from eight evacuation centres in the district moved to the gymnasium of the Greenpia Hotel, which had not been damaged by the tsunami. On 2 April, families with family members who required nursing care were moved to guest rooms in the hotel (total 250 people). Evacuation facilities at the Greenpia gymnasium were closed on 20 June when temporary accommodation became available.
In the district prior to the disaster, people were concerned about their blood pressure and many measured their blood pressure at home. Therefore automated sphygmomanometers were installed at the Greenpia evacuation centre. Evacuees with high blood pressure presented for health consultation at the clinic for blood pressure management.
From 14 March to 26 August, one to three doctors aided the medical management efforts of our clinic per my instructions: (1) one doctor was originally from this area (14 March to 27 March); and (2) physicians belonging to organizations such as Médecins Sans Frontières (MSF) (21 March to 27 May), the Japanese Association of Cardiovascular Intervention and Therapeutics and the Japanese Circulation Society assisted on a rotational basis (18 April to 26 August).
Health care workers from Shimonoseki (Figure 1) were dispatched from 1 April to the end of July. They undertook the health management of evacuees at the evacuation centres and temporary housing facilities. Psychological care was provided by other teams.
Many medical goods requested by the clinic were sent from within and outside the country. In particular, MSF donated medical products, equipment and resources (logisticians and an architect) for the new temporary clinic.
By 19 April, post-mortems had been carried out on 140 bodies in the Taro District. The identities of all the bodies found were confirmed, except one person who died in a fire. I undertook post-mortems on 100 of the 140 bodies and considered the cause of death in almost all cases to be from crushing and/or drowning.
No gastrointestinal or respiratory infection clusters were observed while the evacuation centres were open, nor were there any reports of thromboembolism. No emergency appeals were made to the evacuation centres after the medical evaluation on 13 May.
Table 1 identifies the major diseases that our clinic and the MSF medical team detected from day 10 to day 70 after the earthquake. Data from day 10 (21 March) to day 20 (31 March) reflected the number of cases treated by the MSF medical team who visited each evacuation centre. From day 21 (1 April) the number of cases who visited the temporary clinic at Greenpia is shown.
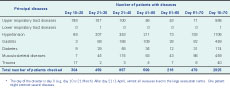
* The day of the disaster is day 0 (e.g. day 10 is 21 March). After day 21 (1 April), almost all evacuees lived in the large evacuation centre. One patient might contract several diseases.
After people transferred from the small evacuation centres to larger ones with higher ceilings on 1 April, the incidence of sporadic upper respiratory tract diseases cases appeared to fall (Table 1). However, it appeared that several lifestyle-related diseases (e.g. hypertension, diabetes) cases increased after transfer to the larger evacuation centre.
The situation remained stable as more people moved into temporary housing in mid-May. By the end of July the evacuation centres closed and all evacuees (an estimated total of 1200 people) had moved to temporary houses. Following this, health management could be undertaken based on the personal responsibility of individuals, as it had been before the disaster.
From late March to mid-May 2011, 130 support personnel, more than 80% of the total, received psychological interviews, which contributed to the psychological stability of those individuals. Following this, there were continued consultations with persons wishing to have them and continuous management of at-risk persons.
There were reports of suicides among staff at the City Office at the nearby disaster area, but in the Taro District there were no such instances. As of November 2011 there had been no cases of attempted suicide or deaths of people living alone, but with many people having emotional trauma, continuing psychological care is being undertaken.
As the only physician in the sole municipal health facility in a rural area under disaster setting, I performed: (1) safe evacuation; (2) disease prevention activities in evacuation centres; (3) psychosocial care for evacuees and relief workers; (4) setting up a temporary clinic, including procurement of medical equipment; (5) medical care at evacuation centres/temporary clinics; (6) staff management, including medical/mental care; (7) liaison with local government and external organizations; and (8) post-mortems. I have described my disaster-related experiences to highlight three relevant factors from World Health Organization documents regarding disaster preparedness and response:11 disaster-resilient health facilities, community capacity and advocacy/awareness.
In Japan the official average number of physicians is 22.5 per 10 000 people, while in Iwate Prefecture it is 19.2 and in Miyako City it is 12.0.1 Our area has fewer physicians compared with Japan’s average, and I am the only physician working with a population of 4434 in the Taro District. Limited medical capacity in a rural area had both advantages and disadvantages in the disaster scenario.
The staff of the clinic knew all the patients and their families very well. This made it easier to maintain relationships with patients and to respond promptly to their needs (e.g. triage, emergency prescription without medical records). This close relationship was also helpful for continuous medical care and preventative measures to be carried out in the evacuation phase.
The disadvantage of limited medical capacity is that staff can become overwhelmed as a result of the sudden increased workload when they themselves are also victims of disaster. There was a clear need for backup medical support. Management of medical products and goods and communication with the district government or media was time consuming given the limited capacity. Maintenance of health and medical activities will not occur through medical personnel alone, but also requires mutual aid between citizens, officers, logisticians and the cooperation of people.
Backup systems for medical charts or prescription histories which are resilient to massive damage are very important to maintain continuity of medical care. We were able to recover partial information that was stored in a non-affected computer server. A backup system should be part of a package of disaster-resilient medical information technology systems in the future. In addition, clinics should be located away from tsunami areas, balancing location with the convenience of patients.
Various medical organizations came to inspect and evaluate the disaster zone after the earthquake. It would perhaps have been better if a disaster support personnel dispatch centre had been set up immediately to coordinate the deployment of support personnel. In addition, the medical teams from outside the district were not familiar with the local medical care. External support staff should be briefed on the local situation in advance of providing medical support. Nonetheless, the support personnel who were active in the district for this event had a valuable learning experience and can contribute expertise in responding to future disasters.
Since I started working in Taro 10 years ago, our clinic has emphasized the importance of blood pressure control given the high prevalence of hypertension in the local population, and we have been working to implement automatic blood pressure measurement at home. In the evacuation centres, evacuees frequently used the automated sphygmomanometers installed. Evacuees with high blood pressure came for health consultations or attended the clinic; blood pressure management thus proved to be a springboard for enabling further health management.
It is also believed that the active participation of evacuees in radio gymnastic exercises was one of the preventive measures against disease including thromboembolism. People cooperated with infection prevention measures and infectious diseases did not become prevalent. This illustrated the mutual trust that existed between health care personnel and citizens.
After people left the larger evacuation centre, the incidence of upper respiratory tract diseases appeared to decline. Given that most respiratory tract infections are spread via droplet transmission, additional space in the temporary accommodation may have reduced the opportunity for transmission and contributed to this decline. In addition, the diffusion and dilution of the pathogens would likely be more dispersed as result of better humidity and ventilation management in the temporary accommodation compared to the evacuation centres. Furthermore, the fact that the evacuees were 10 km from the disaster zone meant that the frequency of contact with rubble and polluted sludge decreased.
It appeared that the number of hypertension and diabetes patients increased after people relocated to Greenpia. One possible reason for this increase was that people visited the clinic for prescriptions of routine medications, including those used to treat hypertension and diabetes. In addition, during this period, more people received routine medical care than before and so existing diseases were more often identified. Stress and imbalance of calorie intake and exercise may worsen these diseases.
At the evacuation centre, it is possible that the manifestation of and/or deterioration in lifestyle-related diseases such as diabetes, hypertension and obesity, was the result of diet and lack of exercise. Meals were provided by the government and were not specific to individual needs. Insufficient exercise during day-to-day life, which might have been exacerbated by most people losing their jobs, also may have been a factor. In addition to addressing infection control in evacuation centres, it may be beneficial to manage the diet and exercise routines of evacuees to maintain health condition.
The neighbourhood associations that existed before the disaster should be re-established as soon as possible to ensure a mutual assistance framework among citizens (e.g. encouraging appropriate exercise or food intake, voluntary supportive mechanisms for the elderly).
There are many populated regions in the world where earthquakes can occur and disasters are likely to result. It is crucial to think carefully about what should be done when disaster strikes. Evacuation drills are important as are evaluating post-disaster needs of securing lifeline services and means of communication, the maintenance of people’s day-to-day lives in the evacuation centres, the assessment of the whereabouts of citizens and the means for the continued provision of medical services.
It is believed that approximately 30 to 40 minutes passed between the earthquake and the tsunami. There were few survivors of the tsunami in the Taro District.
I am proud to have contributed to post-mortems as an important process of grief care for family members of the deceased. However, I want to emphasize again the importance of immediate evacuation after such an earthquake to limit the number of tsunami-related deaths.
This report is a descriptive study with the inherent limitations based on personal experience. However, I hope that this experience will be used for disaster-resilient health system development.
None declared.
None.