a Hunter New England Population Health, New South Wales, Australia.
Correspondence to Julie K Kohlhagen (e-mail: Julie.Kohlhagen@hnehealth.nsw.gov.au).
To cite this article:
Kohlhagen J et al. eeting measles elimination indicators: surveillance performance in a regional area of Australia. Western Pacific Surveillance and Response Journal, 2011, 2(3):5-9. doi:10.5365/wpsar.2011.2.2.008
The World Health Organization (WHO) Western Pacific Region has established specific measles elimination surveillance indicators. There has been concern in Australia that these indicators may be too stringent and that measles elimination can occur without all surveillance prerequisites being met, in particular the minimum fever and rash clinician-suspected measles reporting rate with subsequent laboratory exclusion of measles. A regional public health unit in northern New South Wales, Australia, prompted local general practitioners to report fever and rash presentations that met the measles case definition or that they considered to be clinical measles. These notifications from July 2006 to June 2008 were reviewed to determine whether measles indicators for monitoring progress towards measles elimination could be achieved in Australia. Results confirmed that the surveillance indicators of “>2 reported suspected measles cases per 100 000 population,” “at least 80% of suspected cases adequately investigated within 48 hours” and “greater than 80% of cases had adequate blood samples collected” could be met. Only half the cases had virology that would allow genotyping of measles virus. Special efforts to engage and convince Australian medical doctors about the public health value of reporting clinically suggestive measles cases and collecting confirmatory blood tests resulted in the current WHO Western Pacific Region indicators for progress towards measles elimination being met in a regional area of Australia.
Measles is a highly infectious viral illness that caused an estimated 164 000 deaths worldwide in 2008.1,2 As humans are the only natural host of measles virus, there is only a single genetically stable serotype, there is a safe and effective vaccine that provides long-lasting protection, and indigenous measles transmission has been interrupted in the Region of the Americas since 2002, global measles eradication is considered feasible and desirable.3 The World Health Organization Western Pacific Regional Committee has established a measles elimination target date of 2012.3
Measles continues to occur in Australia with most cases in recent years resulting directly from importation of the virus. In 2009 and 2010, there were 105 and 69 confirmed measles cases notified in Australia, respectively.5 Australian researchers claim that measles has been eliminated based on: absence of endemic measles genotype (D1) since 1999; high vaccination coverage (measles–containing vaccine [MCV] first dose coverage >95% and MCV2 coverage >90% since 2004); serological evidence of >90% population immunity and containment of outbreaks without apparent re-establishment of a specific genotype since 1999.6,7 The contention is that despite not meeting all Western Pacific Region surveillance targets at the national level there is adequate evidence to justify formal declaration of measles elimination in Australia.7
However, during 2011 there has been an increase in measles activity with 82 cases reported to 31 March, with most cases locally acquired without clear epidemiological links apparent between all cases.5 An average of 69 measles cases were reported in New South Wales (NSW) each year for the past 10 years.5 We reviewed suspected measles cases reported between July 2006 and June 2008 in a regional area of northern New South Wales to determine whether the Western Pacific Region indicators for monitoring progress towards measles elimination were met at the subnational level and what implications there might be for documenting sustained elimination in Australia. During the study period 2006–2008, measles notification rates in Australia were 0.1–0.6 per 100 000 population.5
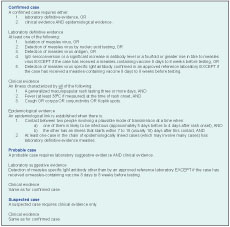
Surveillance data on measles is collected in New South Wales under the requirements of the Public Health Act (2010). All patient presentations meeting the measles clinical case definition of the National Notifiable Diseases Surveillance System are required to be reported by doctors, hospital chief executive officers, laboratories, school principals and directors of child care facilities (Box 1).8
Hunter New England is located in northern New South Wales and has a total population of 880 000. The Public Health Unit regularly prompts local general practitioners to report fever and rash presentations that meet the measles case definition or that they consider to be clinical measles. All suspected measles notifications to the local Public Health Unit are routinely recorded in a secure dedicated Microsoft Excel 2007 spread sheet, and information on probable and confirmed cases is entered into the NSW Notifiable Conditions Information Management System. Suspected measles cases reported by clinicians were analysed to determine whether they met the clinical case definition for measles notification (Box 1).8 Additional surveillance data were used to determine the likelihood of measles, including travel out of the area or overseas, exposure to other known measles cases and immunization status, with individuals considered fully immunized if they were age-appropriately immunized with MCV1 and MCV2.9 Timing of response, laboratory test requests and results were also reviewed.
This surveillance project was classified as a quality assurance project by the Hunter New England Health Research Ethics Committee.
The Public Health Unit received 63 suspected measles notifications during the study period July 2006 to June 2008, and 48 had specimens collected either before notification or after discussion with the Public Health Unit. Notifications were received from general practitioners, pathology laboratories, child care centres, schools and health services.
In addition one young child visiting the area from Europe with his family was reported by a general practitioner after the child presented with fever, maculopapular rash, cough, lethargy, coryza and conjunctivitis. Serology, available within 24 hours of collection, confirmed measles. PCR results were available within seven days and genotype D8 was identified. A total of 161 contacts were identified, with normal human immunoglobulin administered to eight and measles vaccine to 19. No secondary cases were identified.
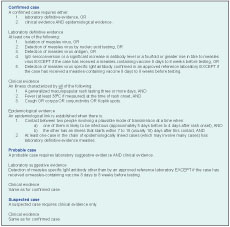
Of the 63 reported suspected cases, 15 cases were excluded immediately because they did not have clinical features consistent with the measles definition. Forty-eight cases had clinical or epidemiological evidence suggestive of measles at the time of notification to justify collection of pathology specimens. The main presenting symptom for notification of suspected measles was rash (100% of notified cases) (Table 1). On further investigation some of the rashes were not consistent with a measles rash and not all suspected cases had fever at rash onset. Only three suspected cases fulfilled the National Notifiable Diseases case definition.
Fifty-nine measles diagnostic specimens were collected for the 48 suspected cases and only one case had measles confirmed (measles IgM and PCR both positive). Forty-two of the 48 cases (87.5%) had serology collected for measles IgM and IgG. Seventeen had urine and nasopharyngeal swabs submitted for PCR. In addition to measles and rubella testing, parvovirus was tested in five suspected measles cases and not detected. Notification of suspected measles cases occurred from one day before specimens were collected to six days after specimens were collected, with the median being less than one day after the specimens were collected. The median time between notifications of suspected cases to receiving a laboratory result was two days.
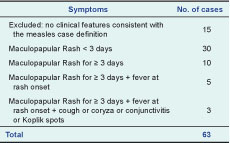
For the 48 suspected measles cases with specimens collected, 11 were less than 12 months of age and not yet immunized. Thirty-seven cases had immunization status recorded and of these 26 were age-appropriately immunized against measles while three were not age-appropriately immunized (Table 2). Among those not immunized, two were children of conscientious objector parents, and one child was born overseas and not fully immunized according to the Australian schedule.
The project was undertaken during a period where published immunization rates for the study area were: 93.6% of children aged 12 to 15 months (MCV1) and 91.3% of children aged 72 to 75 months (MCV2).11
The area met six of the 10 Western Pacific Region interim measles elimination indicators (Table 3); two were not applicable as no clusters were identified and one indicator was not applicable as the regional area is a single district. Immunization coverage fell short of the 95% indicator.

* Adequate investigation: collection of essential data elements (date of rash onset, date of specimen collection, vaccination status, date of last vaccination, date of birth or age, sex, district) and search for epidemiologically-linked cases.10
Our results confirmed that the surveillance indicators of “>2 reported suspected measles cases per 100 000 population,” “at least 80% of suspected cases adequately investigated within 48 hours” and “greater than 80% of cases had adequate blood samples collected” that had not previously been reported at the national level in Australia could indeed be achieved at the subnational level.6 As quality surveillance indicators have been met and high immunization coverage has been maintained in this regional area, it is likely that indigenous measles has been eliminated.
Clinicians were often convinced, on the basis of limited clinical features, that a patient had measles. The reliability of clinical diagnosis alone will become progressively insecure as measles becomes increasingly uncommon. A high level of alertness at the primary care level is essential if early detection of imported and secondary cases is to be achieved in an area that has eliminated indigenous measles transmission.12 Current clinician awareness in this regional area appears adequate.
The review highlighted the need to gather thorough epidemiological information, risk exposure and immunization history when suspected measles cases are reported. A low threshold for serological or virological testing is required if suspected measles cases are to be excluded as confirmed cases. In Victoria, Australia, specimens negative for measles-specific IgM are routinely tested for rubella and parvovirus B19-specific IgM.13 The absence of an endemic measles genotype for at least 12 months has been suggested as an important alternative measure of measles elimination.7 Only half of the suspected cases had specimens collected for measles genotyping, so applying this endemic measles genotype measure will be difficult if the suspected cases became confirmed cases.
Immunization coverage in Australia has been at 91–92% since the end of 2003 for the 24 month age group while those in the six year age group remain below 90%.9 Meeting the 95% Western Pacific Region immunization target will be difficult. It then becomes important to meet the Western Pacific Region quality surveillance indicators for building the evidence that Australia has eliminated measles.14
Since the study period, suspected measles notifications have continued at the same rate, and four cases in the study area have been confirmed as measles; all were imported from overseas or other parts of Australia. No secondary cases have occurred and no endemic measles genotype has been isolated.
As Western Pacific Region measles elimination approaches, it is important that all countries achieve the surveillance targets necessary for confirming interruption of indigenous measles transmission, including demonstrating their ability to rapidly investigate and exclude cases meeting the clinical case definition. We found that special efforts to engage and convince Australian medical doctors about the public health value of reporting clinically suggestive measles cases and collecting confirming blood tests resulted in the current Western Pacific Region indicators for progress towards measles elimination being met in a regional area of Australia.
None.