Seroprevalence survey
To determine the proportion of asymptomatic infections, voluntary blood sampling was carried out in 2007 in the three largest clusters of cases at Bukit Batok, Woodlands and Pasir Ris, where all household members residing in each site were invited to participate. A recruitment and sampling site was set up within each of the clusters to take blood samples (3 ml) and to conduct face-to-face interviews. Only residents who gave written consent were interviewed. Individuals whose serum samples contained anti-DENV IgM were scored as having a recent infection and those whose serum samples contained anti-DENV IgM but could not recall any recent symptoms of dengue infection were classified as asymptomatic.16
Statistical analysis
Microsoft Office Excel 2007 and SPSS 15.0 were used for statistical analyses. Differences between the age-gender-standardized incidence rates were computed and tested for statistical significance using the Z-test.17 Statistical significance was taken at P < 0.05 level.
Ethics
The study was conducted primarily as part of a national public health programme, with supplemental data obtained from a community seroprevalence study which had been approved by the National Environment Agency Bioethics Review Committee (IRB 005.2) in 2007.
Results
Epidemiological findings
A total of 8826 laboratory-confirmed cases of dengue were reported in 2007, an incidence rate of 192.3 per 100 000 population. Of these, 8637 (97.9%) were DF and 189 (2.1%) were DHF. Twenty-four fatalities were reported in 2007, comprised of eight DF and 16 DHF cases, a case-fatality rate (CFR) of 0.27% for all dengue cases and 8.5% for all DHF cases, comparable to the outbreak in 2005. In 2005, 27 fatalities were reported, comprising three DF and 24 DHF cases, a CFR of 0.19% for all dengue cases and 6.1% for all DHF cases.10 The outbreaks in 2005 and 2007 differed in that 257 cases of DF/DHF were reported in January 2007, far fewer than the 1262 cases reported in the same period of 2005.10 Most cases (1633) were reported in July 2007, two months earlier than the peak of 2770 cases that were reported in September 200510 (Figure 1).
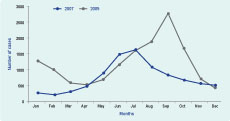
Figure 1. Monthly distribution of dengue cases in 2005 and 2007
The median age of DF/DHF cases among Singapore residents in 2007 was 37 years (interquartile range 25 to 50), with a range from two days to 101 years, higher than the median age of 31 years (interquartile range 20 to 42), with a range from four days to 98 years, in 2005.10 The age-specific incidence rate for dengue was highest in the age group 55 years and above in 2007. In 2005, it was highest in the 15 to 24-year-old age group (Table 1).10
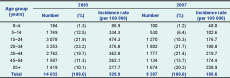
Table 1. Age-specific incidence rates of reported indigenous cases of dengue, Singapore, 2005 and 2007
The incidence in males was significantly higher than in females (209.3 per 100 000 and 150.3 per 100 000, respectively) and that was true for all ethnic groups (P < 0.01). Among Singapore residents in 2007, the age-gender-adjusted incidence rate of DF/DHF was highest in the Chinese (172.3 per 100 000) (P < 0.01), followed by the Malays (146.9 per 100 000) (P < 0.05) and the Indians (120.9 per 100 000). Among Singapore residents in 2005, the age-gender-adjusted incidence rate of DF/DHF was also highest in the Chinese (312.8 per 100 000) followed by the Malays (288.4 per 100 000) and the Indians (173.9 per 100 000).10
The incidence rate in 2007 was highest among those residing in private condominiums (453.8 per 100 000), and was 1.3 times that of those residing in compound houses (351.1 per 100 000) and almost three times that of those residing in high-rise public housing apartments (156.5 per 100 000). This was different from 2005 when the lowest rate (298.8 per 100 000) was found in residents of private condominiums, while the incidence rate of those residing in compound houses was 710.7 per 100 000, and 332.1 per 100 000 for those living in high-rise public housing apartments.10
Cases were concentrated in the urban and suburban centres of the central (29.0%) and south-eastern (20.4%) parts of Singapore, with further geographical extension to the western suburban areas (Figure 2). A total of 3877 cases from 949 clusters (median three cases, range two to 117 cases) were identified. The total number of cases from reported clusters constituted less than half (46.8%) of all reported cases.

Figure 2. Geographical distribution of Aedes albopictus, Aedes aegypti and dengue cases, Singapore, 2005 and 2007
The largest clusters were at Bukit Batok (117 cases, July to September), Pasir Ris (71 cases, May to July) and Woodlands (67 cases, July to August). Two of these localities (Woodlands and Bukit Batok) also were affected in 2005, but with fewer cases.10 The seroprevalence study involving 1708 residents conducted in these three localities revealed that 3.3% (n = 56) had recent dengue infections. Among these residents with recent infection, 73.2%, ranging from 57.1% at Woodlands to 81.8% at Pasir Ris, did not recall any symptoms within the previous three months.
Virological findings
All four dengue virus serotypes circulated in Singapore from 2005 to 2007. The predominant serotype circulating in 2005 was DENV-1,10 but in January 2007 it was overtaken by DENV-2, which re-emerged with a clade replacement,14 and has since remained the predominant serotype (Figure 3). In 2007, RNA from 1044 confirmed cases of acute dengue infection were serotyped/strong> at the EHI, NEA, Department of Pathology, Singapore General Hospital and the laboratories at Tan Tock Seng Hospital and National University Hospital, and comprised 88.3% DENV-2, 6.4% DENV-1, 4.6% DENV-3 and 0.7% DENV-4.
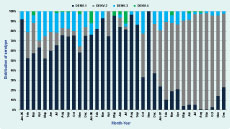
Figure 3. Dengue virus serotypes identified at Environmental Health Institute, Department of Pathology, Singapore General Hospital and laboratories at Tan Tock Seng Hospital and National University Hospital, Singapore, 2005–2007
Entomological findings
As in 2005, the distribution of dengue cases in 2007 was more closely associated with Aedes aegypti than with Aedes albopictus breeding sites (Figure 2).10 The overall Aedes premises index was 0.68% in 2007, lower than the 1.15% observed in 2005.10
The top three breeding habitats for Aedes aegypti in 2005 and 2007 were similar, with domestic containers (26% in 2005, 32% in 2007), ornamental containers (24% in 2005, 21% in 2007) and flower pot plates (7% in 2005, 11% in 2007) constituting more than half of all breeding habitats.10 However, for Aedes albopictus, there was a decrease in the number of breeding sites found in discarded receptacles (from 21% in 2005 to 4% in 2007).10
Discussion
With the exception of median age of the cases, and the predominant dengue serotype, the epidemiological features of the 2007 epidemic were largely similar to those of 2005. The increase in median age and the finding that those aged more than 55 years had the highest incidence are poorly understood. It is interesting to note that this phenomenon has accompanied the switch to DENV-2, and both the phenomenon and predominance of DENV-2 have persisted till 2010.
After the 2005 outbreak, the dengue control system was enhanced going into 2007. First, manpower that routinely carried out Aedes surveillance and source reduction was increased from 250 in 2005 to about 500 in 2007. On average, 116 764 residential premises and 3011 non-residential premises (e.g. construction sites, schools) were inspected every month in 2007, resulting in almost all premises being inspected within the year.13 Second, an intensive source reduction exercise was conducted by NEA officers two to three months before the expected dengue season, to remove breeding and potential breeding grounds. Third, early warnings systems were developed through virological surveillance and ambient temperature monitoring, providing temporal risk stratification.14 Lastly, qualitative spatial risk stratification was performed using case, virus and larva surveillance data, to guide the deployment of staff. Despite the enhanced vector control which led to a premises index of 0.68%, which was significantly lower than the 2.24%, 1.7% and 2% found from 2002 to 2004 (when the same cosmopolitan genotype DENV was predominant), respectively, an outbreak still ensued.
Phylogenetic analyses of DENV-2 envelope gene sequences at EHI, NEA, revealed that the switch in predominant serotype in early 2007 coincided with a clade replacement within DENV-2. Within the Cosmopolitan genotype of DENV-2, there were two distinct subclades with strong temporal topology. The old clade was detected from 2000 to 2005 and the new clade from 2007 to 2008.14 The role of the small genetic changes between the two clades, in viral fitness, is being investigated. A similar observation was reported in Cuba, where the authors hypothesized that the 1997 severe outbreak in Cuba was a result of a small mutation that improved the fitness of DENV-2.18
The epidemiology of dengue in Singapore has evolved from a paediatric problem in the 1960s to an adult infection since the 1980s. The median age has shifted from 14 years in 1973,19 to 37 years in 2007. This has been attributed to the lower transmission rate, which was demonstrated by a mathematical model that showed a declining trend in the force of infection (defined as per capita rate at which susceptible individuals in the community acquire infection)20 since the nationwide vector control programme was first implemented in the late 1960s.
Previous studies have demonstrated that more than 90% of dengue infections were asymptomatic.21 In a survey representative of the adult general population conducted in 2004, the prevalence of asymptomatic infections was found to be 95%.22 The prevalence of asymptomatic dengue infections in surveys conducted during the 2007 outbreak in three public housing estates ranged from 57.1% to 81.8%. The differences could be due to different methodologies.
A limitation on this study would be the reliance on notification data. The incidence rate is actually the case notification/detection rate. Although medical practitioners and directors of clinical laboratories were required to report all cases of DF/DHF to the Ministry of Health, mild cases with undifferentiated fevers may not seek medical care and so may not be reported. The actual incidence of dengue infection in 2007, therefore, could be higher than was reported. A limitation of the seroprevalance survey was that convenience sampling was done, and data collected may not be representative of the population. Nevertheless, it gives us an idea of the prevalence of asymptomatic infections in these outbreak areas.
The 2007 dengue epidemic in Singapore demonstrated the dynamic interactions of the virus, human host, vector and the environment, as evidenced by the resurgence caused by introduction of a new clade of DENV-2, despite sustained vector control efforts. Given the large estimated proportion of asymptomatic infections, the real extent of the problem could be much larger than what is currently known. Singapore remains vulnerable to major outbreaks of dengue through the constant introduction of viruses from travellers; and through local evolution of the virus.
Conflicts of interests
None declared.
Funding
None.
References:
- Halstead SB. Pathogenesis of dengue: challenges to molecular biology. Science, 1988, 239:476–81. doi:10.1126/science.3277268 pmid:3277268
- Sabin AB, Schlesinger RW. Production of immunity to dengue with virus modified by propagation in mice. Science, 1945, 101:640–642. doi:10.1126/science.101.2634.640 pmid:17844088
- Dengue: guidelines for diagnosis, treatment, prevention and control – New edition. Geneva, World Health Organization, 2009.
-
Suaya JA et al. Cost of dengue cases in eight countries in the Americas and Asia:
a prospective study. The American Journal of Tropical Medicine and Hygiene, 2009, 80:846–855. pmid:19407136 - The Dengue Strategic Plan for the Asia Pacific Region 2008–2015. New Delhi (SEARO) and Manila (WPRO), World Health Organization, 2008. Available from: http://www.wpro.who.int/NR/rdonlyres/F7EE04BF-0B31-4BB3-B99F-CF482D24A7C7/0/dengue_plan.pdf [accessed 28 February 2011].
- Goh KT et al. Epidemiological aspects of an outbreak of dengue fever/dengue haemorrhagic fever in Singapore. The Southeast Asian Journal of Tropical Medicine and Public Health, 1987, 18:295–302. pmid:3433161
-
Epidemiology of dengue fever/dengue haemorrhagic fever. World Health Organization, World Epidemiological Report, 1990, 65:101–118. Available from: http://whqlibdoc.who.int/wer/WHO_WER_1990/WER1990_65_101-108%20
(N%C2%B014).pdf [accessed 28 February 2011]. - Ministry of Health, Committee of Epidemic Diseases. Surveillance of dengue fever/dengue haemorrhagic fever, 1992. Epidemiological News Bulletin(Singapore), 1993, 19:13–17.
- Ministry of Health, Singapore Committee of Epidemic Diseases. Dengue surveillance in Singapore, 1998. Epidemiological News Bulletin(Singapore), 1999, 25:1–3.
- Koh BK et al. The 2005 dengue epidemic in Singapore: epidemiology, prevention and control. Annals of the Academy of Medicine, Singapore, 2008, 37:538–45. pmid:18695764
- Goh KT, Ong A, Low J, editors. A guide on infectious diseases of public health importance in Singapore, 6th ed. Singapore, Ministry of Health and Tan Tock Seng Hospital, 2004.
- Lai YL et al. Cost-effective real-time reverse transcriptase PCR (RT-PCR) to screen for Dengue virus followed by rapid single-tube multiplex RT-PCR for serotyping of the virus. Journal of Clinical Microbiology, 2007, 45:935–941. doi:10.1128/JCM.01258-06 pmid:17215345
-
Tang CS et al. Surveillance and control of dengue vectors in Singapore. Epidemiological News Bulletin, 2006, 32:1–9. Available from: http://www.moh.gov.sg/mohcorp/uploadedfiles/Publications/ Epidemiological_News_Bulletin/2006/ENB01Q_06.pdf [accessed
28 February 2011]. - Lee KS et al. Dengue virus surveillance for early warning, Singapore. Emerging Infectious Diseases, 2010, 16:847–9. pmid:20409381
- Singapore Resident Population 2003–2008. Singapore, Department of Statistics, 2009.
- Yew YW et al. Seroepidemiology of dengue virus infection among adults in Singapore. Annals of the Academy of Medicine. Singapore, 2009, 38:667–675. pmid:19736569
- Armitage P, Berry G. Statistical Methods in Medical Research, 2nd ed. Oxford, Blackwell Scientific, 1987.
- Rodriquez-Roche R et al. Virus role during intraepidemic increase in dengue disease severity. Vector-Borne and Zoonotic Diseases, 2011, 11:00.
- Goh KT. Changing epidemiology of dengue in Singapore. Lancet, 1995, 346:1098. doi:10.1016/S0140-6736(95)91771-3 pmid:7564804
- Egger JR et al. Reconstructing historical changes in the force of infection of dengue fever in Singapore: implications for surveillance and control. Bulletin of the World Health Organization, 2008, 86:187–96. doi:10.2471/BLT.07.040170 pmid:18368205
-
Goh KT. Seroepidemiology of dengue virus infection in Singapore.
In: Goh KT (ed). Singapore, Ministry of the Environment, 1998, 50–72. - Ye T et al. Seroprevalence study on past and recent dengue virus infection in Singapore. Epidemiological News Bulletin (Singapore), 2007, 33:36–41.