a Communicable Diseases Division, Ministry of Health, College of Medicine Building, 16 College Road, Singapore 169854.
b Veterinary Public Health Laboratory Division, Agri-Food & Veterinary Authority of Singapore, 10 Perahu Road, Singapore 719937.
c Department of Pathology, Singapore General Hospital, Outram Road, Singapore 169608.
d Food Control Division, Agri-Food & Veterinary Authority of Singapore, 5 Maxwell Road, Tower Block, MND Complex, Singapore 069110.
e Office of the Director of Medical Services, Ministry of Health, College of Medicine Building, 16 College Road, Singapore 169854.
Correspondence to Suhana Binte Solhan (e-mail: suhana_solhan@moh.gov.sg).
To cite this article:
Suhana et al. An outbreak of Salmonella enterica serotype Enteritidis traced to cream cakes. Western Pacific Surveillance and Response Journal, 2011, 2(1):23-30. doi:10.5365/wpsar.2010.1.1.001
Introduction: This paper describes the epidemiological, microbiological and environmental investigations conducted during an outbreak of Salmonella gastroenteritis in Singapore.
Methods: A case-control study was undertaken to identify the vehicle of transmission. Microbiological testing was performed on faecal, food and environmental samples. Isolates of Salmonella were further characterized by phage typing and ribotyping.
Results: There were 216 gastroenteritis cases reported from 20 November to 4 December 2007. The causative agent was identified as Salmonella enterica subspecies enterica serotype Enteritidis for 14 out of 20 cases tested. The vehicle of transmission was traced to cream cakes produced by a bakery and sold at its retail outlets (P < 0.001, OR = 143.00, 95% Cl = 27.23–759.10). More than two-thirds of the 40 Salmonella strains isolated from hospitalized cases, food samples and asymptomatic food handlers were of phage type 1; the others reacted but did not conform to any phage type. The phage types correlated well with their unique antibiograms. The ribotype patterns of 22 selected isolates tested were highly similar, indicating genetic relatedness. The dendrogram of the strains from the outbreak showed distinct clustering and correlation compared to the non-outbreak strains, confirming a common source of infection.
Discussion: The cream cakes were likely contaminated by one of the ingredients used in the icing. Cross-contamination down the production line and subsequent storage of cakes at ambient temperatures for a prolonged period before consumption could have resulted in the outbreak.
Salmonella enterica subspecies enterica serotype Enteritidis (Salmonella Enteritidis) is one of the most common Salmonella serotypes worldwide, particularly in developed countries.1 Its increasing incidence in the United Kingdom and the United States of America in the 1980s was mainly attributed to consumption of raw or undercooked contaminated poultry, hen eggs and egg-containing products.2,3 In Asia, Salmonella Enteritidis has also emerged as the most common human serotype in Japan, the Republic of Korea and Thailand.4 In Singapore, it accounted for 62.2% of human non-typhoidal salmonelloses in 2007.5 The vehicles of transmission identified in a few reported localized outbreaks included luncheon pork6 and an egg-based Malay pancake.7
We undertook extensive epidemiological, microbiological and environmental investigations during an outbreak of Salmonella gastroenteritis in November and December 2007 in Singapore to determine the causative agent, source of infection and mode of transmission.
On 23 November 2007, the Singapore Ministry of Health was notified of an outbreak of food poisoning involving 15 people who developed illness within 48 hours after attending a birthday celebration. In the following weeks, other clusters of cases were reported from different parts of Singapore. Preliminary investigation showed that most of the cases had consumed cream cakes purchased from various retail outlets that were franchisees of a large and well known local bakery. No other type of cake or bakery products was implicated.
In view of the unusual occurrences of gastroenteritis suspected to be linked to the bakery and with onset of symptoms since 20 November, outbreak control measures were concurrently implemented while epidemiological investigations were in progress. The public was educated and alerted to the outbreak through the media and advised to discard all bakery products purchased from the implicated retail outlets. Joint actions were taken by the Singapore Ministry of Health; the Agri-Food & Veterinary Authority of Singapore, the licensing authority of the bakery; and the National Environment Agency, the licensing authority of the retail outlets. The bakery was ordered to recall all cream cakes from distribution and sale on 30 November 2007. Production of cream cakes ceased on 3 December followed by other bakery products on the next day. Both the bakery and retail outlets were subsequently closed on 4 December and 5 December, respectively, for thorough cleaning and disinfecting. The last case reported onset of illness on 4 December.
All cases reporting symptoms consistent with the case definition between 20 November and 8 December were interviewed and relevant clinical and epidemiological data such as age, sex, ethnicity, clinical symptoms, date of onset of illness, food items eaten 72 hours before onset of illness, food establishments visited and medical treatment sought were obtained. A case reported during this period was defined as a person who developed diarrhoea (two or more liquid stools per day) and one or more of the following symptoms: nausea, vomiting or abdominal cramps. Contact tracing was also conducted to search for unreported cases.
A case-control study was initiated to determine the specific vehicle(s) of transmission. We made an attempt to obtain more epidemiological information from the first 60 consecutive cases that fit our case definition and from about 100 controls. Interviews were conducted using a set of structured questionnaires to find out what food had been consumed 72 hours before onset of illness and who had contact with pets or family members with history of diarrhoea within the last seven days. Controls consisted of apparently healthy individuals with no recent travel history or gastrointestinal symptoms during the previous two weeks. They were asked similar questions covering the period within three weeks of onset of illness of the reported cases.
Differences in proportions between cases and controls were compared using χ2 test or Fisher’s exact test. To quantify the extent of risk, odds ratio and its 95% confidence interval were also derived. All calculations were performed using SPSS version 15 (SPSS Inc., Chicago, IL). A P value of < 0.05 was considered to be statistically significant in a two-tailed test.
All food handlers and staff in the bakery, including delivery men, cleaners and staff in the 38 retail outlets were referred for a medical examination that included testing of stool samples for enteric pathogens. Raw ingredients, food samples and environmental swabs were sent for microbiological analyses.
The methods for the culture of Salmonella and other bacterial enteropathogens from stools and food samples have been described in previous outbreak investigations.6 Fresh 24-hour Salmonella isolates grown on blood agar plates were serotyped by slide agglutination with antisera obtained from Statens Serum Insitut of Copenhagen, Denmark.8 Isolates of Salmonella Enteritidis were further analysed by biotyping (antimicrobial susceptibility testing), phage typing and molecular typing (ribotyping). Antimicrobial susceptibility testing was performed using a disk diffusion method on Mueller Hinton agar and Clinical and Laboratory Standards Institute interpretive criteria,9 while phage typing was carried out by the method of Ward et al.10
Automated ribotyping was performed with isolates from the cases, food samples and food handlers in the outbreak, as well as isolates not related to the outbreak (food samples and ATCC type strain). Automated ribotyping was performed with the RiboPrinter microbial characterization system (RP) (Qualicon, Inc., DuPont, Wilmington, DL). The isolates were cultured on blood agar consisting of trypticase soy agar and 5% sheep blood (BBL Microbiology Systems, Cockeysville, MD) and incubated overnight at 35 °C. Colonies were picked from individual culture plates, placed in tubes containing lysis buffer, heat treated and loaded into the RP. Within the RP, bacterial DNA digestion was accomplished with 50uL of PstI at 40 U/uL (Roche Diagnostics GmbH, Mannheim, Germany) and 50uL of SphI at 40 U/uL (Roche Diagnostics GmbH, Mannheim, Germany). The substitute restriction enzyme protocol in which digestion takes place at 37 °C for two hours was used. The Riboprint pattern for each isolate was then compared to the patterns generated for the other isolates. Interpretation of the ribotype patterns was aided by use of the software BioNumerics 2.5 (Applied Maths, Sint-Martens-Latem, Belgium) and the use of an import script provided by DuPont-Qualicon to import the patterns into BioNumerics. Clustering was performed by using the unweighted pair-group method with arithmetic averages based on Pearson correlation (global pattern comparison). A dendrogram was constructed with the BionNumerics software. Clustering was performed by using a 1% optimization parameter and a 1% band position tolerance.
Site visits were made to the suspected bakery and its retail outlets to identify the possible sources and causes of contamination. The entire production process in the bakery from the purchase of raw ingredients to distribution in the retail outlets was thoroughly reviewed with the management.
The investigations were carried out in accordance with the Infectious Diseases Act of Singapore.
A total of 39 reports of food poisoning occurring either singly or in small clusters involving 216 people that met the case definition were reported, with onset of illness between 20 November and 4 December 2007 (Figure 1). The main presenting symptoms were diarrhoea (96%), fever (63%), vomiting (60%) and headache (16%). Their ages ranged from one year to 78 years (median age, 29 years) with no gender difference. Among the major ethnic groups in Singapore, Chinese comprised 70.4% of the cases; Malays, 27.3%; and others, 2.3%. Of the reported cases, 18 (8.3%) were hospitalized while the rest either sought outpatient treatment or self-medicated.
Of the first 60 cases contacted, 54 agreed to participate. We attempted to enrol approximately 100 controls however only 39 agreed to participate. Results of the case-control study based on 54 cases and 39 controls implicated cream cakes from the suspected bakery (P < 0.001, OR = 143.00, 95% CI = 27.23–759.10) as the vehicle of transmission (Table 1). No other food items or risk factors were implicated. The median incubation period based on the interval between consumption of the implicated food item and onset of illness was 12.3 hours (range: 3–139 hours).
* Purchased from suspected confectionary and its retail outlets
A total of 428 faecal specimens from cases (20), and food handlers (176) and retail outlet staff from the bakery (232) were tested for bacterial enteropathogens. Salmonella Enteritidis was isolated from 14 (70%) of 20 cases. Six (3.4%) of 176 food handlers and staff from the bakery and four (1.7%) of 232 staff from the retail outlets also tested positive for Salmonella Enteritidis. Three other food handlers (two from the factory, one from a retail outlet) were positive for Salmonella Group C and another food handler (from another retail outlet) for Salmonella Group E.
Seventy raw ingredients, 25 semi-processed products and five ready-to-serve products from the factory were tested. Of these 100 samples, 12 semiprocessed products and ready-to-serve products (whole hazelnuts from an opened container, one truffle chocolate cream specimen, two chocolate cream specimens and eight hazelnut paste specimens taken from different opened tubs) tested positive for Salmonella Enteritidis. One food sample showed high bacterial count (Standard Plate Count = 160 000 000 cfu/gm) and another tested positive for Bacillus cereus. Of 23 ready-toserve products from nine of 38 retail outlets, eight cake samples from five of the outlets also tested positive for Salmonella Enteritidis with a concomitant high bacterial count (Standard Plate Count = 4 300 000 cfu/gm). Of two cake remnants provided by the cases, one was positive for Salmonella Enteritidis and the other for Salmonella Group C.
All the environmental swabs were negative for Salmonella. A raw egg sample taken from the house of one hospitalized care and raw and liquid eggs obtained from the supplier of the bakery were negative for Salmonella.
Phage typing results of isolates from the food handlers, food samples and cases showed 27 (67.5%) out of 40 isolates were of phage type 1 and 13 (32.5%) were isolates that reacted but did not conform (RDNC) (Table 2). The phage type correlated well with the antibiogram results, with the strains within each phage type having a unique antibiogram. Salmonella Enteritidis of both phage type 1 and RDNC isolates were sensitive to ampicillin, chloramphenicol, ceftriaxone and ciprofloxacin and resistant to nalidixic acid. Salmonella Enteritidis phage type 1, however, was resistant to sulphamethoxazole/ trimethoprim while that of RDNC isolates were sensitive to it.
Ribotyping using PstI and SphI restriction enzymes for restriction of DNA showed that the ribotype patterns obtained were highly similar between isolates, indicative of direct genetic relatedness between the isolates even though they are of a different phage type (Figure 2). The dendrogram from the cluster analysis showed the distinct clustering and correlation of the Salmonella Enteritidis isolates from the outbreak as compared to the non-outbreak strains (Figure 3).
Semi-processed products and ready-to-serve food items were not adequately separated. Utensils and working surfaces were also not cleaned and disinfected thoroughly and regularly. High-risk food ingredients such as cream produced in bulk quantity were left at ambient temperatures for prolonged periods. Moreover, the final ready-to-serve products were not immediately kept in refrigerators with temperature display to prevent bacterial growth. No irregularities in personal and food hygiene among the food handlers were observed during the site visits. None of the staff reported recent history of gastrointestinal illness.
Butter cream was a key ingredient used to make the cream cakes. It was processed in-house, unlike the production of other types of cakes in which ready-to-add packaged fresh cream was used. The butter cream was made from butter, sugar syrup that had been boiled at high temperature (120 °C) and half-whisked egg whites. The egg whites were manually separated from the whole eggs by the production staff who claimed that they were properly gloved during the process. After being cracked and their contents separated, these eggs were pooled in the kitchen and held at room temperature. Other ingredients such as chocolate paste or hazelnut paste were subsequently mixed with the butter cream to form chocolate cream or hazelnut cream, respectively. The butter cream was prepared in bulk quantity for use over two production days. The prepared creams were stored at room temperature in the production area. The prepared creams were used to sandwich the chocolate sponge bases that had been baked in the oven. The final product was then decorated. The cakes and other bakery products were delivered from the bakery to 38 retail outlets around the island in well maintained refrigerated trucks in accordance to specified schedules. The cakes at the retail outlets were displayed for sale in well maintained refrigerated showcases.
This outbreak was the largest common source outbreak of gastroenteritis caused by Salmonella enterica subspecies enterica serotype Enteritidis in Singapore. The epidemiological evidence implicating cream cake as the vehicle of transmission was supported by microbiological and molecular findings. Salmonella serotype Enteritidis was isolated from cases, food samples and food handlers. More than two-thirds of the isolates belonged to phage type 1, and the others reacted, but did not conform to any phage type. Although the phage type correlated well with the antibiogram findings, with the strains within each phage type having a unique antibiogram, the ribotype patterns among the isolates (phage type 1 and RDNC) were highly similar, indicating genetic relatedness. Moreover, the dendrogram of the Salmonella Enteritidis isolates from the outbreak showed distinct clustering and correlation compared to the non-outbreak strains. The multiple laboratory methods enabled us to discriminate the Salmonella strains isolated from various sources and link the outbreak to a common source.11,12
Cakes, ice cream and other bakery products (e.g. custards) are known vehicles of transmission of Salmonella Enteritidis and ingredients made from raw eggs provided a potential source of contamination.13–17 Ingredients made from raw eggs provide a potential source of contamination In this outbreak, egg white manually separated from raw egg yolks was one of the ingredients of the butter cream processed in-house for the icing of cream cakes. The eggs were not pasteurized or heated to a high temperature, unlike other ingredients of the icing. The exact mechanism by which the implicated cake was contaminated remained unclear. We could not rule out the possibility of introduction of Salmonella Enteritidis via a particular batch of eggs sent to the bakery before the outbreak, although egg samples taken from the supplier were negative. Ready-to-serve cream cakes, kept in the open preparation area uncovered at ambient temperatures in the bakery for at least two hours before distribution by refrigerated trucks to the retail outlets, could have led to further multiplication of Salmonella to high infective doses.
The asymptomatic food handlers who tested positive for Salmonella Enteritidis could have been infected during preparation, handling or consumption of contaminated cream cakes during the outbreak. Some of these workers at the bakery were routinely assigned to break the eggs to obtain the egg white or taste-test the quality of the ingredients, while others claimed to have eaten the implicated cakes. Infected food handlers can transmit Salmonella organisms to food ingredients, work surfaces and utensils, if personal and food hygiene practices are insufficiently observed.18–21 Salmonella Enteritidis has been recovered from fingers following the breaking of intact shell eggs artificially contaminated with the enteropathogen, with some organisms surviving hand-washing with soap and hot water.21
Cross-contamination of utensils, equipment and work surfaces could have also occurred as the layout of the cake production area was such that semi-processed products and ready-to-serve food items were not adequately segregated. Salmonella can survive in the environment for several days.22 Cross contamination down the production line could also have caused the food products and whole hazelnuts (opened packet) to be contaminated.
There were several limitations in the epidemiological investigations of this outbreak. In the case-control study, the number of controls was too few as some who were identified refused to participate in the interview. This resulted in the wide confidence intervals of the implicated food item. Also, the questionnaires did not include other food items that either used raw eggs as an ingredient or were manufactured by other bakeries, even though it was unlikely that any of these food items would be the vehicle of transmission, and the respondents had difficulty recalling all the food items consumed. Furthermore, we did not know the shelf life of the cream cakes, batch numbers and the quantities manufactured, which could have been used to explain, to some extent, the transmission of infection.
We had no evidence to implicate raw eggs used forthe icing as the source ofinfection, as no Salmonella could be isolated from the samples tested. Thus, we could not explain how the semi-processed and ready-to-serve products became contaminated in the factory. The hazelnuts could have been contaminated at the source since they did not undergo heat treatment in the bakery. However, a trace back investigation was not conducted. Additionally, detailed information regarding poultry flocks and eggs was not available. Lastly, in this outbreak, less than 10% of the reported cases had their stools examined for Salmonella organisms as most of them either self-medicated or were treated as outpatients.
Notification of cases from this outbreak was based on both reports of food poisoning and routine reporting of infections with Salmonella. In view of several local outbreaks that were caused by Salmonella, reporting of Salmonella in Singapore was subsequently made mandatory in 2009. This will enable more rapid and targeted epidemiological investigations into common source foodborne outbreaks of salmonellosis.
This outbreak highlighted the importance of prompt notifications of food poisoning incidents by clinicians, clinical laboratories and the public. As soon as the vehicle of transmission was suspected, the public was quickly alerted and immediate action taken to recall and destroy the implicated products and temporarily halt production, as in other reported outbreaks.23 The availability of routine molecular typing techniques in outbreak settings would facilitate tracing the source of infection and confirming epidemiological linkages of the Salmonella strains isolated from humans, food, animals and the environment. The incident also served as a good reminder to all food handlers to constantly observe proper personal and food hygiene practices. Food manufacturers are also advised to use only pasteurized eggs for food products that do not undergo severe heat treatment.
This article is based on a report from Communicable Disease Surveillance in Singapore, 2007. Reference: Outbreak of Salmonellosis traced to consumption of cream cakes, Communicable Disease Surveillance in Singapore, 2007, Singapore: Ministry of Health; 2008. Available from: http://www.moh.gov.sg/mohcorp/uploadedFiles/Publications/
None declared.
There was no specific funding for the investigation. Cost incurred was borne by the Ministry of Health, Singapore (under the Surveillance and Outbreak Investigation Financial Vote).
We would like to thank the staff from Surveillance & Response Branch, Singapore Ministry of Health, the Food Control Division, AVA and the Regional Offices, NEA, for their assistance in the investigation and control of this outbreak. We would also like to thank the laboratory personnel from the various laboratories for their support.
Erratum: A spelling error was corrected and the titles of the axes of the graph were added for Figure 1 on 31 March 2011.
Table 2. Results of phage typing of isolates of Salmonella Enteritidis
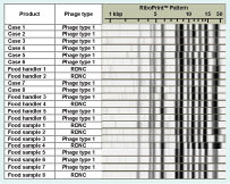
Figure 2. Results of phage typing and ribotyping of Salmonella Enteritidis isolates from eight cases, six food handlers and eight food samples

Figure 3. Dendogram of Salmonella Enteritidis isolates using automated ribotyping
Environmental investigation
Discussion
Note:
Reports/2008/Special%20Feature.pdf.
Conflicts of interest
Funding
Acknowledgements
References:
6:1–9.
4:24–26.
2006–2007. Morbidity and Mortality Weekly Report, 2007, 56:521–524.
pmid:17538526