|
Free Neuropathology 1:12 (2020) |
|
Review |
|
Top ten discoveries of the year: Neurodegeneration |
|
John F. Crary |
|
Neuropathology Brain Bank & Research CoRE, Department of Pathology, Nash Family Department of Neuroscience, Ronald M. Loeb Center for Alzheimer's Disease, Friedman Brain Institute, Icahn School of Medicine at Mount Sinai, New York, NY, USA |
|
Corresponding author: |
|
Submitted: 26 January 2020 Accepted: 02 April 2020 Copyedited by: Nima Sharifai Published: 08 April 2020 |
|
Keywords: Neurodegeneration, Neuropathology, Alzheimer’s disease, Limbic-predominant age-related TDP-43 encephalopathy, Amyotrophic lateral sclerosis, Parkinson’s disease, Huntington’s disease |
|
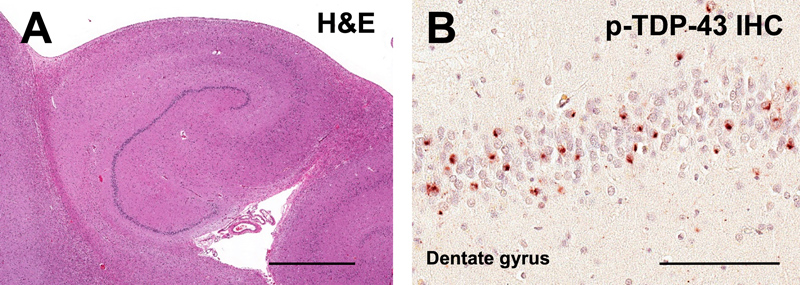
Abstract As we embark on a new year of scientific inquiry in neurodegenerative disease research, it is helpful to take a look back and consider the contributions in the field with the potential to be the most impactful. The purpose of this review is to highlight recent advances in 2019 which have the potential to be transformative in the field of neurodegenerative neuropathology. Substantive scientific progress rarely occurs as a “eureka moment”, and when possible, we opted to highlight collaborative efforts and research trends. We also included groundbreaking methodologies and tools. The generous increases in federal funding in the United States and elsewhere have massively expanded the total number of active programs researching Alzheimer’s disease. This exacerbates an imbalance, and an effort was made to highlight innovations across disease categories, and not to permit dementia to crowd out movement disorders, motor neuron disease, ataxias, etc. Thus, our overall goal was to highlight some of the most important discoveries, tools or methods that we feel will most likely directly enhance our ability to understand and diagnose neurodegenerative brain diseases. Given space limitations and the targeted readership of this journal, we selected ten topics most relevant to neuropathologists and clinical neuroscientists: 1. A new neurodegenerative disease category, 2. A new approach to probing gene expression on the single cell level, 3. A new approach merging histology and gene expression profiling, 4. A new computational approach using deep machine learning and computer vision, 5. A neuropathological substrate for sleep disturbance in Alzheimer’s disease, 6. A candidate pathogenic agent for Alzheimer’s disease, 7. A comprehensive approach to morphometric analysis of cerebellar neurodegeneration, 8. The strongest evidence yet linking neurodegeneration to contact sports, 9. Mounting evidence for gut to central nervous system transmission in Parkinson’s disease, and 10. A spotlight on glia in Huntington’s disease. 1. LATE, a new old neurodegenerative disease As the population ages, researchers are gleaning fundamental new insights from the oldest-old population (i.e., those over the age of 80 years) whose vulnerability to neuropathology diverges from the younger-old. In a paper published in Brain, a large group of neuropathologists led by Dr. Peter Nelson at the University of Kentucky introduced a new diagnostic category, limbic-predominant age-related TDP-43 encephalopathy (LATE), describing a type of neurodegeneration that mostly strikes elderly individuals over 80 years old (Nelson et al., 2019). This work was the culmination of many years of study and a consensus group report, the goal of which was to address how to deal with the surprisingly large number of patients that variably develop an amnestic dementia that is very similar to that seen in Alzheimer’s disease (AD), but with abnormalities in the transactive response DNA binding protein of 43 kDa (TDP-43). Historically, the first study to recognize that there was something different occurring in these patients did so by identifying 13 autopsied subjects with dementia who had marked neuronal loss with reactive gliosis in the medial temporal lobe, but had no Alzheimer’s neuropathological changes; this was termed “hippocampal sclerosis” (Dickson et al., 1994). This neuropathological signature is not specific, and it was not until TDP-43 was discovered in amyotrophic lateral sclerosis (ALS) and frontotemporal lobar degeneration (FTLD) patients that investigators thought to also look in hippocampal sclerosis patients and ultimately link the two. It was also recognized that subjects with TDP-43 proteinopathy only variably present with a pattern histologically considered hippocampal sclerosis on hematoxylin and eosin (H&E) stain. Neuropathologically, subjects with LATE have the tell-tale abnormal translocation of TDP-43 from the nucleus to the cytoplasm, where it becomes phosphorylated (Figure 1). In LATE, TDP-43 pathology can be detected in numerous brain regions, some of which overlap with FTLD, but the amygdala is most severely affected, followed by the hippocampal formation. Nelson et al. provided diagnostic criteria and a proposed hierarchical staging system for assessing patients for LATE neuropathologic change: TDP-43 immunohistochemistry is essential (hippocampal sclerosis pathology only is not sufficient) and should be performed in the amygdala (stage 1), mid-level hippocampus (stage 2) and middle frontal gyrus (stage 3).
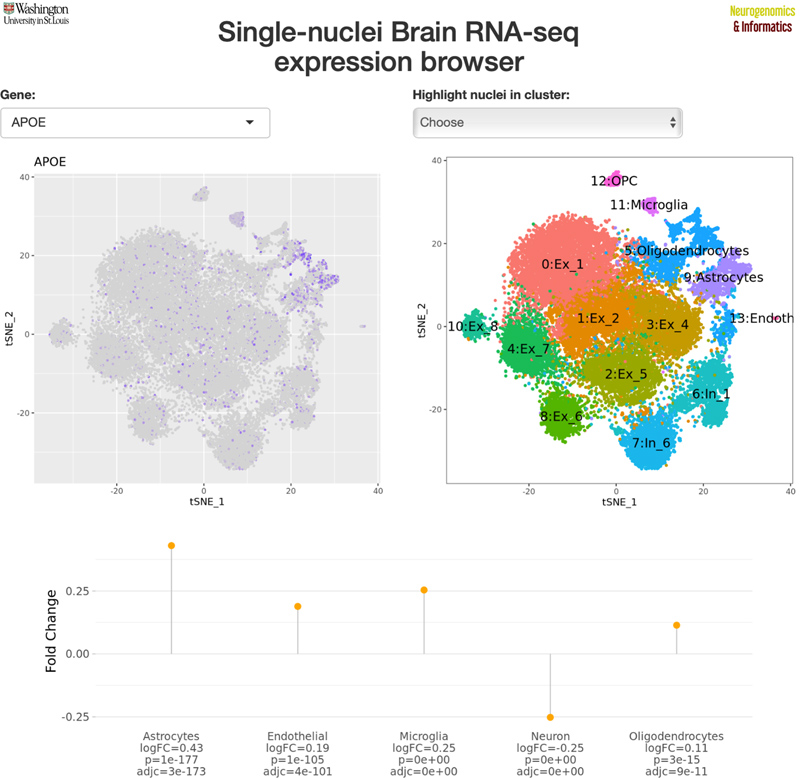
Figure 1. Limbic-predominant age-related TDP-43 encephalopathy (LATE). (A) LATE neuropathological change in an 83-year-old woman with dementia and the clinical diagnosis of AD. Marked atrophy and neuronal loss in the hippocampal formation, but with minimal AD neuropathological change. (B) TDP-43 proteinopathy is shown in the dentate gyrus. Image courtesy of Dr. Peter Nelson (NIH grant P30 AG028383). There is a great deal that we have to learn by studying LATE. While a few genes have been implicated as risk factors (i.e., APOE, GRN, TMEM106B, ABCC9, KCNMB2), larger genetic studies have the potential to better delineate mechanisms and causal pathways that could serve as biomarkers and therapeutic targets. Further, we have very little understanding of the extent to which LATE affects non-Caucasian populations; studying more diverse populations has the potential to expand on risk factors, genetic and otherwise. Biochemical and molecular studies of TDP-43, including secondary modifications such as phosphorylation, have the potential to lead to biomarkers that could be used pre-mortem. Finally, co-morbidities are nearly universal in the oldest-old population, and the extent to which they interact with LATE pathology will be important for understanding its clinical significance. 2. Single-cell transcriptomics Nothing has plagued molecular profiling of post-mortem neurodegenerative disease brain tissue more than the problem of normalization in the context of variable and often massive neuronal loss with commensurate reactive gliosis. Numerous approaches have been developed to address this problem (e.g., deconvolution of bulk RNA sequencing or expression profiling of pooled cells isolated by laser capture microdissection), but they are laborious and results often fall short. Recent advances in high-throughput single cell sorting using microfluidics coupled with next-generation sequencing have enabled a paradigm shift in how gene expression profiles can be investigated. The first papers deploying single-cell RNA sequencing (scRNA-seq) in human post-mortem neurodegenerative disease tissues have emerged in 2019 and we expect this to transform transcriptomic studies (Del-Aguila et al., 2019; Grubman et al., 2019; Mathys et al., 2019). One of the major barriers that investigators encountered in applying single cell technology to human post-mortem brain is that it is not possible to isolate single cells from frozen tissue given the membrane breakdown. Thus, scRNA-seq is currently best done from cells isolated from fresh brain tissue, and precludes using archival frozen banked brains. Previous work in animal models, however, has shown that single nuclei can withstand the freezing process and yield nuclear RNA profiles that can serve as a proxy for those generated from cytoplasmic RNA. Because of this, groups are focusing on this variant approach termed single nuclei RNA-seq (snRNA-seq, or just Nuc-Seq). Three studies were published in 2019 using Nuc-Seq in post-mortem human brain tissue from patients with neurodegenerative disease. In the first, published online in August by Del-Aguila et al, investigators at Washington University in Saint Louis used Nuc-Seq to profile a patient with the PSEN1 p.A79V mutation and compared it to two related family members with sporadic AD (non-mutational), and proposed a collection of best practices (Del-Aguila et al., 2019). All of these studies have made the data available online (Figure 2). In November, Grubman et al., from Monash University (Australia) and Duke-National University of Singapore Medical School, examined the entorhinal cortex from 6 sporadic patients and 6 controls. Their group found that AD is associated with downregulation of APOE in oligodendrocyte precursors and astrocytes, and with upregulation of APOE in a subpopulation of microglia. They also explored transcription factor regulatory modules (Grubman et al., 2019). Finally, in the largest study published in June by Mathys et al., investigators at the Broad Institute of MIT/Harvard profiled the prefrontal cortex from 48 individuals from the Rush ROSMAP cohort and identified sex differences in disease-associated subpopulations of cells, and found interesting recurrent differences in myelination that might play a role in AD (Mathys et al., 2019). Together, these results are the first step towards providing a highly detailed cell-type specific molecular atlas of neurodegenerative diseases.
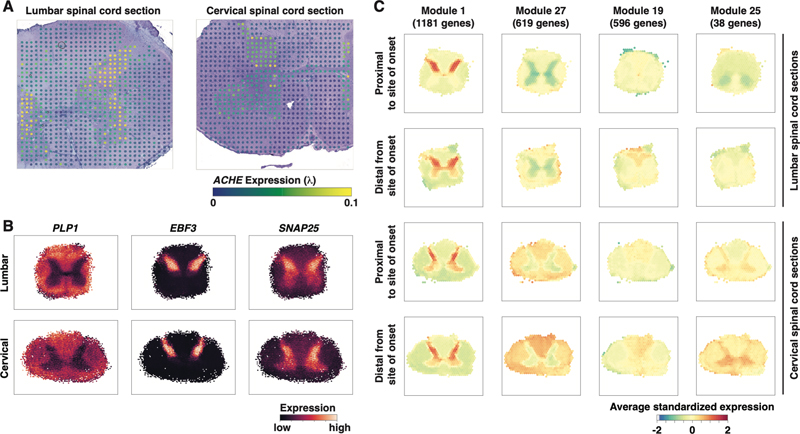
Figure 2. Single-nuclei RNA-seq (snRNA-seq) brain expression browser. Cell type specific expression profiles can be shown using a publicly available interactive web-based resource (http://ngi.pub/snuclRNA-seq). 3. Spatial transcriptomics Essentially all approaches to measuring gene expression are limited by the fact that isolation of nucleic acids from tissue by necessity disrupts the spatial relationship of the cells of interest. Losing the cellular architecture is a major barrier to understanding the context of genome-wide changes in RNA expression. This year we saw the first use of spatial transcriptomics, a method first introduced in 2016 that bridges RNA-sequencing and histopathology by allowing researchers to generate thousands of gene expression profiles from a single histological section using a slide printed with an array of barcoded specialized mRNA-capturing probes (Ståhl et al., 2016). In a study led by Hemali Phatnani at the New York Genome Center and published in Science (Maniatis et al., 2019), spatial transcriptomics was applied to post-mortem human amyotrophic lateral sclerosis tissue from seven patients with either lumbar- or bulbar-onset sporadic ALS (Figure 3). They also profiled SOD1-G93A transgenic mice. Together, they quantitated the spatial distribution of 11,138 mouse and 9624 human genes in spinal cord sections and confirmed the alteration in expression of some known ALS genes. They were also able to identify an abnormal microglial signature that preceded astroglial dysfunction. They chose to follow up on a mechanism involving TREM2 and its partner TYROBP, revealing a spatiotemporal ordering with TYROBP expression upregulated pre-symptomatically before TREM2. Changes in other genes that are part of this mechanism (e.g., APOE, CX3CR1, LPL, B2M and CX3CR1) occurred later. These results demonstrate how this technology can lead to novel insights by being deployed as part of an interdisciplinary approach to neurodegenerative disease.
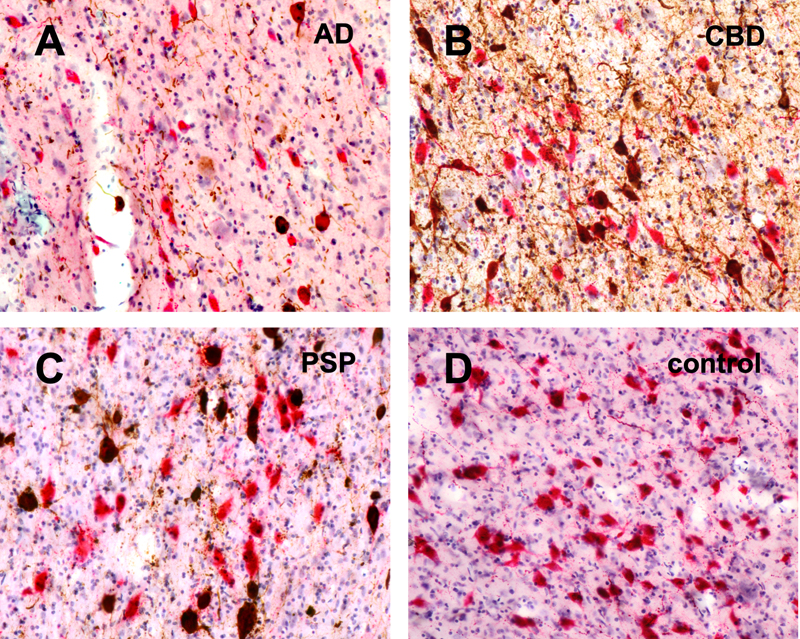
Figure 3. Identification of expression programs using spatially resolved transcriptomics. (A) Example data for a single gene from Spatial Transcriptomics profiling of postmortem lumbar and cervical spinal cord sections from a sporadic ALS patient presenting with bulbar symptom onset. (B) Data from many Spatial Transcriptomics arrays were aligned to a common coordinate system, and expression levels were hex binned spatially. This procedure enables reconstruction of larger regions than can be profiled with a single array and reveals expected spatial expression patterns for genes expressed by cell types present in specific tissue domains. (C) Spatially resolved coexpression analysis reveals gene sets with tissue domain specific expression patterns, a subset of which also exhibit differences with respect to proximity to the site of symptom onset. Figure courtesy of Drs. Hemali Phatnani and Silas Maniatis. 4. Artificial intelligence and computer vision Since Alois Alzheimer first described the disease that bears his name in 1906, revealing striking morphological changes using ammoniacal silver stains, there has been very little progress in the way these cellular changes are interpreted. Visual microscopic examination remains state-of-the-art, but it is slow, imprecise, marginally reproducible and requires the experience of a highly trained neuropathologist, the numbers of which are dwindling. The task is highly repetitive and fatigue inducing, which increases the likelihood of error. The whole process would be best suited to automation, but the concept of a machine that could substitute for a neuropathologist seemed implausible until recent developments in the field of artificial intelligence. Increases in computational power combined with improved algorithms for training artificial neural networks have placed us at the precipice of a transformation moment in neuropathology. The most common machine learning approach to analyzing visual imagery is the convolutional neural network (CNN). These are a type of deep learning, a class of artificial neural networks with multiple layers that progressively extract more complex features from the input. CNNs are based on the architecture of the organization of the animal visual cortex, encompassing simulations of overlapping receptive fields what were described by Hubel and Wiesel in the cat and monkey in the 1950s and 1960s. This year we saw the first two papers deploying deep learning to analyze digital whole slide images from patients with neurodegenerative diseases to identify both amyloid plaques and neurofibrillary tangles. One paper, published in Nature Communications and led by Dr. Brittany Dugger (University of California Davis), reported a deep learning pipeline that identifies amyloid plaques and cerebral amyloid angiopathy in immunohistochemically stained slides (Tang et al., 2019). To build this, they annotated over 70,000 plaques that served as ground truth to train and evaluate the CNN achieving 0.993 receiver operating characteristic (ROC) curve and 0.743 precision recall curve. In another paper, investigators from the Center for Computational and Systems Pathology at the Icahn School of Medicine at Mount Sinai, led by Dr. John F. Crary (author of this review) and published in Laboratory Investigation, focused on neurofibrillary tangle pathology (Signaevsky et al., 2019). This study used 3177 images derived from patients with primary age-related tauopathy, chronic traumatic encephalopathy, progressive supranuclear palsy and Alzheimer’s disease to train and test the network, achieving recall, precision and F1 scores of 0.91, 0.80 and 0.85 respectively. We expect that this approach will be transformative in the near future with the development of sophisticated neural networks capable of rapidly and reproducibly analyzing slides alongside, or perhaps instead of, the neuropathologist. In the long term, this will certainly transform the skillset of the neuropathologist, who will perhaps be less adept at picking up subtle morphological features by eye, but hopefully more able to deploy computational and other modern tools. 5. A neuropathological substrate for sleep-wake disruption in Alzheimer’s disease Sleep-wake disruption is common in aging and associated with cognitive decline and decreased quality of life. Sleep disturbance is seen in a number of neurodegenerative diseases and is amongst the earliest symptoms of AD. This includes reduced total, slow wave, and rapid eye movement (REM) sleep time. There are arousal deficiencies, including daytime sleepiness, that can precede cognitive impairment. Competition between subcortical populations of both wake promoting neurons (WPNs) and sleep promoting neurons (SPNs) provide a switch that coordinates sleep behaviors. Among these populations, WPNs in the locus coeruleus, orexin/hypocretin-producing neurons in the lateral hypothalamic area, and histaminergic neurons in the tuberomammillary nucleus (TMN) play critical roles in stimulating the cerebral cortex and contributing to arousal. The neuropathological substrate for sleep disturbances in AD remains unclear, but attention has been focused on amyloid-beta (Aβ) as sleep promotes its clearance. Accumulation of abnormal hyperphosphorylated tau (p-tau), however, is a stronger correlate of neurodegeneration and functional decline, and accumulation of p-tau in WPNs is among the first AD neuropathological changes to appear in the brain. In a powerful study published in Alzheimer’s & Dementia, a team led by Dr. Lea Grinberg (UCSF) directly addressed the question of p-tau pathology in brainstem WPNs in AD by performing rigorous quantitative study, using stereological measures of wake-promoting cells in the locus coeruleus, lateral hypothalamic area and tuberomammillary nucleus in AD, compared to two amyloid-independent primary tauopathies (progressive supranuclear palsy and corticobasal degeneration) and healthy controls (Oh et al., 2019). They found that while all three of these diseases displayed the presence of p-tau in WPNs, only the AD patients exhibited clinically relevant cell loss (Figure 4). The implications are that loss of these cells are an important component of sleep disturbance in AD, but also that amyloid-independent tauopathies may benefit from alternative clinical approaches (e.g., suppression of the arousal system).
Figure 4. Tau pathology in the locus coeruleus in Alzheimer’s disease compared to progressive supranuclear palsy, corticobasal degeneration and controls. Double-label immunohistochemistry showing colocalization of tau pathology (brown) and norepinephrine (red). Figure courtesy of Dr. Lea Grinberg. 6. Periodontal disease as a risk factor for Alzheimer’s disease Neuroinflammation is a well-recognized feature of AD, with activation of microglia, inflammasomes, and complement. Over the years, a number of infectious agents have been postulated to trigger this inflammation and participate in disease pathogenesis. The Aβ peptide itself has even been demonstrated to have antimicrobial properties, supporting this hypothesis. One candidate pathogenic agent that has emerged is Porphyromonas gingivalis, a pathogen that plays a critical role as a keystone pathogen in chronic periodontitis (CP). Previously, among other supportive data, P. gingivalis was shown to be associated with cognitive decline in AD patients compared to controls without CP. Furthermore, oral infection of Apoe-/- transgenic mice resulted in brain infection and complement activation. In a paper published in Science Advances, researchers led by Drs. Jan Potempa (University of Louisville) and Stephen S. Dominy (Cortexyme) have provided the strongest evidence yet that infiltration of the brain with P. gingivalis might be causal and that their toxicity is through their virulence factors termed gingipains (Dominy et al., 2019). Gingipains are secreted cysteine proteases that play critical roles related to host colonization, inactivation of host defenses, iron/nutrient acquisition, and destruction of tissue. These researchers demonstrated the presence of gingipains in post-mortem AD brain tissue alongside the presence of P. gingivalis DNA. Remarkably, treatment with a small molecule gingipain inhibitor blocks gingipain-induced neurodegeneration in an animal model with an associated decrease in host Aβ response to P. gingivalis. This orally available gingipain inhibitor is currently being tested in human clinical studies. More work needs to be done, and it is anticipated that this work might trigger a new research trend around periodontal disease in AD. 7. Deconstructing cerebellar degeneration using “patholog-omics” Essential tremor (ET) is a common condition that can be associated with significant morbidity. For many years, the neuropathological features underlying ET had been a complete mystery, with autopsy studies being limited and qualitative. Recently, investigators have been building large cohorts of ET patients and a series of ET-related neuropathological changes have been reported, but many had been observed in other neurodegenerative diseases affecting the cerebellum, raising questions of specificity. How these features and the other cerebellar degenerations are related had never been formally or systematically studied. In what could be considered a tour de force, investigators led by Drs. Elan Louis (Yale University) and Phyllis Faust (Columbia University) published as landmark paper in Acta Neuropathologica applying what they termed a “patholog-omics” approach using 37 quantitative morphological metrics (Louis et al., 2019). They compared 156 brains from healthy controls and patients with a spectrum of cerebellar diseases, including essential tremor, spinocerebellar ataxia, multiple system atrophy, Parkinson’s disease, and dystonia, mapping unique cellular patterns of neurodegeneration. Measures included Purkinje cell loss, axonal changes (e.g., torpedoes), basket cell hypertrophy, climbing fiber synaptic changes and others. They then used principal component analysis to derive distinctive and overlapping signatures marking each of these disorders. This study, which is the first of its kind to attempt to apply “omics” approaches to histomorphology, paves the way towards applying the approach to other neurodegenerative diseases. 8. Chronic traumatic encephalopathy and American football: a dose-response relationship While the fact that repetitive mild traumatic brain injury leads to devastating long-term sequelae in professional boxers has been recognized for close to a century without controversy, chronic traumatic encephalopathy (CTE) only recently began to achieve substantial scientific scrutiny and public interest when it was identified in American football players. While there is strong evidence that repetitive head injuries are causal for CTE, skeptics remain. Among the criticisms is that while clinicopathological studies are powerful, they are association analyses that ostensibly cannot prove a causal relationship on their own. This is not the whole story. In 1965, Sir Austin Bradford Hill, an English statistician, proposed nine criteria that, when met, provide epidemiologic evidence of causality. In terms of CTE, eight of these criteria had been met, including strength (effect size), reproducibility, specificity, temporality, plausibility, coherence, experimentation and analogy. The missing criterion, until now, was evidence of a biological gradient: the presence of a dose-response relationship showing that increased exposure leads to a greater incidence/magnitude of the effect. In a report published online in November 2019 in the Annals of Neurology, researchers led by Drs. Jesse Mez and Ann C. McKee (Boston University) measured exposure to contact sports in the largest autopsy series of American football players ever assembled and calculated CTE risk. They found that the odds of CTE doubled with every 2.6 years of American football played (Mez et al., 2020). This paper firmly establishes that there is a dose-response relationship between exposure to American football and CTE, which the strongest indicator of causality obtainable. This study also provides hard data for athletes and families trying to determine how much exposure might be considered safe. 9. Parkinson’s disease: the gut-brain connection The pathological spread of abnormal protein aggregates through “prion-like” templated misfolding is strongly implicated in a host of neurodegenerative diseases. Parkinson’s disease is no exception, with rigorous neuroanatomical studies by Heiko Braak and colleagues describing a hierarchical spread of α-synuclein pathology caudally to rostrally in the central nervous system (Braak et al., 2003). Parkinson’s disease is notable in that it is not restricted to the central nervous system, with α-synuclein aggregates present throughout the body including the gastrointestinal tract. This, together with the fact that the dorsal motor nucleus of the vagus nerve, which heavily innervates the gut, is among the first regions to show α-synuclein pathology, has fueled investigation around whether Parkinson’s disease may be initiated in the gut. This hypothesis is plausible given that a number of cohort studies of human subjects have a reduction in Parkinson’s disease risk following truncal vagotomy. Further, injection of various forms of human or recombinant α-synuclein fibrils into the gut at various sites leads to central pathology, but this pathology was minimal and transient (Holmqvist et al., 2014; Manfredsson et al., 2018; Uemura et al., 2018). Investigators at the Johns Hopkins University School of Medicine published a manuscript in Neuron showing results using a new experimental paradigm, which demonstrated severe and widespread α-synuclein pathology in the brains of transgenic mice following injection of preformed fibrils in the gut (Kim et al., 2019). They injected α-synuclein fibrils directly into the muscularis layer of the duodenum and pylorus and tracked the progression of pathological aggregate generation to the dorsal motor nucleus, caudal hindbrain, and onward to the substantia nigra with accompanying cell loss and functional impairment. Truncal vagotomy blocked this spread, confirming the direct spread through this nerve, confirming what was seen previously. Further, knockout of α-synuclein prevented the spread as well, indicating that the propagation is dependent on the molecule. This new animal model provides a robust experimental system, and together with the previous studies adds to the growing trend focusing on gut to brain transmission in Parkinson’s disease. 10. Huntington’s disease: a spotlight on astrocytes Astrocytes play a critical role in a broad spectrum of nervous system functions, through direct interactions with neurons, blood vessels and other glial cell populations. Thus, it is not surprising that they have been implicated in a number of neurodegenerative disorders. Glial pathology is well-documented in tauopathies (e.g., tufted astrocytes of PSP) and synucleinopathies (e.g., Papp-Lantos bodies in oligodendrocytes in MSA). Huntington’s disease (HD) principally affects the striatum and cortico-striatal-thalamic circuitry with medium spiny neurons being most vulnerable. Intriguingly, the huntingtin gene (HTT) gene is expressed in all cell types, but abnormalities in astrocytes have been demonstrated in post-mortem HD brains tissue. Astrocytes express mutant HTT (mHTT) with increased GFAP expression and reactive changes. Reactive astrocytosis is a constant feature of neurodegeneration that accompanies neuronal loss, but how these changes contribute to disease and the extent to which they are secondary changes or contribute causally is unclear. Emerging evidence from transcriptomic studies has begun to paint a picture suggesting that astrocytes may not be passive bystanders, but may play an active role in some diseases, including HD. These studies have revealed two broad categories of astrocytes, termed A1 and A2, with A1 being neurotoxic (Liddelow et al., 2017; Zamanian et al., 2012). These and other studies prompted a group of investigators at UCLA, led by Dr. Baljit S. Khakh, to take a closer look at astrocytes in HD. Their study, published in October 2019 in Science Translational Medicine, used transcriptomic approaches in post-mortem human brain tissue from 36 Huntington’s disease patients, Vonsattel stage 0-3, alongside two transgenic mouse models to probe astrocyte pathology in HD (Diaz-Castro et al., 2019). In their transgenic animals, they deployed a powerful approach, termed RiboTag, which allowed them to specifically profile RNA expression in astrocytes. The result of this analysis was the elucidation of a novel core disease-associated astrocyte signature consisting of 62 genes seen in both human post-mortem brain and the transgenic animals. Remarkably, alterations in this profile could be ameliorated in their models using transcriptional repression of the mHTT specifically in astrocytes using zinc finger protein (ZFP) transcriptional repressors. These findings are certain to accelerate the intensification of interest in gliobiology in HD and other neurodegenerative disorders. References Braak, H., Del Tredici, K., Rüb, U., de Vos, R. A. I., Jansen Steur, E. N. H., & Braak, E. (2003). Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiology of Aging, 24(2), 197–211. https://doi.org/10.1016/s0197-4580(02)00065-9 Del-Aguila, J. L., Li, Z., Dube, U., Mihindukulasuriya, K. A., Budde, J. P., Fernandez, M. V., Ibanez, L., Bradley, J., Wang, F., Bergmann, K., Davenport, R., Morris, J. C., Holtzman, D. M., Perrin, R. J., Benitez, B. A., Dougherty, J., Cruchaga, C., & Harari, O. (2019). A single-nuclei RNA sequencing study of Mendelian and sporadic AD in the human brain. Alzheimer’s Research & Therapy, 11(1), 71. https://doi.org/10.1186/s13195-019-0524-x Diaz-Castro, B., Gangwani, M. R., Yu, X., Coppola, G., & Khakh, B. S. (2019). Astrocyte molecular signatures in Huntington’s disease. Science Translational Medicine, 11(514), eaaw8546. https://doi.org/10.1126/scitranslmed.aaw8546 Dickson, D.W., Davies, P., Bevona, C., Van Hoeven, K.H., Factor, S.M., Grober, E., Aronson, M.K., Crystal, H.A. (1994) Hippocampal sclerosis: a common pathological feature of dementia in very old (> or = 80 years of age) humans. Acta Neuropathol 88(3), 212–221. https://doi.org/10.1007/bf00293396 Dominy, S. S., Lynch, C., Ermini, F., Benedyk, M., Marczyk, A., Konradi, A., Nguyen, M., Haditsch, U., Raha, D., Griffin, C., Holsinger, L. J., Arastu-Kapur, S., Kaba, S., Lee, A., Ryder, M. I., Potempa, B., Mydel, P., Hellvard, A., Adamowicz, K., … Potempa, J. (2019). Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Science Advances, 5(1), eaau3333. https://doi.org/10.1126/sciadv.aau3333 Grubman, A., Chew, G., Ouyang, J. F., Sun, G., Choo, X. Y., McLean, C., Simmons, R. K., Buckberry, S., Vargas-Landin, D. B., Poppe, D., Pflueger, J., Lister, R., Rackham, O. J. L., Petretto, E., & Polo, J. M. (2019). A single-cell atlas of entorhinal cortex from individuals with Alzheimer’s disease reveals cell-type-specific gene expression regulation. Nature Neuroscience, 22(12), 2087–2097. https://doi.org/10.1038/s41593-019-0539-4 Holmqvist, S., Chutna, O., Bousset, L., Aldrin-Kirk, P., Li, W., Björklund, T., Wang, Z.-Y., Roybon, L., Melki, R., & Li, J.-Y. (2014). Direct evidence of Parkinson pathology spread from the gastrointestinal tract to the brain in rats. Acta Neuropathologica, 128(6), 805–820. https://doi.org/10.1007/s00401-014-1343-6 Kim, S., Kwon, S.-H., Kam, T.-I., Panicker, N., Karuppagounder, S. S., Lee, S., Lee, J. H., Kim, W. R., Kook, M., Foss, C. A., Shen, C., Lee, H., Kulkarni, S., Pasricha, P. J., Lee, G., Pomper, M. G., Dawson, V. L., Dawson, T. M., & Ko, H. S. (2019). Transneuronal Propagation of Pathologic α-Synuclein from the Gut to the Brain Models Parkinson’s Disease. Neuron, 103(4), 627-641.e7. https://doi.org/10.1016/j.neuron.2019.05.035 Liddelow, S. A., Guttenplan, K. A., Clarke, L. E., Bennett, F. C., Bohlen, C. J., Schirmer, L., Bennett, M. L., Münch, A. E., Chung, W.-S., Peterson, T. C., Wilton, D. K., Frouin, A., Napier, B. A., Panicker, N., Kumar, M., Buckwalter, M. S., Rowitch, D. H., Dawson, V. L., Dawson, T. M., … Barres, B. A. (2017). Neurotoxic reactive astrocytes are induced by activated microglia. Nature, 541(7638), 481–487. https://doi.org/10.1038/nature21029 Louis, E. D., Kerridge, C. A., Chatterjee, D., Martuscello, R. T., Diaz, D. T., Koeppen, A. H., Kuo, S.-H., Vonsattel, J.-P. G., Sims, P. A., & Faust, P. L. (2019). Contextualizing the pathology in the essential tremor cerebellar cortex: A patholog-omics approach. Acta Neuropathologica, 138(5), 859–876. https://doi.org/10.1007/s00401-019-02043-7 Manfredsson, F. P., Luk, K. C., Benskey, M. J., Gezer, A., Garcia, J., Kuhn, N. C., Sandoval, I. M., Patterson, J. R., O’Mara, A., Yonkers, R., & Kordower, J. H. (2018). Induction of alpha-synuclein pathology in the enteric nervous system of the rat and non-human primate results in gastrointestinal dysmotility and transient CNS pathology. Neurobiology of Disease, 112, 106–118. https://doi.org/10.1016/j.nbd.2018.01.008 Maniatis, S., Äijö, T., Vickovic, S., Braine, C., Kang, K., Mollbrink, A., Fagegaltier, D., Andrusivová, Ž., Saarenpää, S., Saiz-Castro, G., Cuevas, M., Watters, A., Lundeberg, J., Bonneau, R., & Phatnani, H. (2019). Spatiotemporal dynamics of molecular pathology in amyotrophic lateral sclerosis. Science, 364(6435), 89–93. https://doi.org/10.1126/science.aav9776 Mathys, H., Davila-Velderrain, J., Peng, Z., Gao, F., Mohammadi, S., Young, J. Z., Menon, M., He, L., Abdurrob, F., Jiang, X., Martorell, A. J., Ransohoff, R. M., Hafler, B. P., Bennett, D. A., Kellis, M., & Tsai, L.-H. (2019). Single-cell transcriptomic analysis of Alzheimer’s disease. Nature, 570(7761), 332–337. https://doi.org/10.1038/s41586-019-1195-2 Mez, J., Daneshvar, D. H., Abdolmohammadi, B., Chua, A. S., Alosco, M. L., Kiernan, P. T., Evers, L., Marshall, L., Martin, B. M., Palmisano, J. N., Nowinski, C. J., Mahar, I., Cherry, J. D., Alvarez, V. E., Dwyer, B., Huber, B. R., Stein, T. D., Goldstein, L. E., Katz, D. I., … McKee, A. C. (2020). Duration of American Football Play and Chronic Traumatic Encephalopathy. Annals of Neurology, 87(1), 116–131. https://doi.org/10.1002/ana.25611 Nelson, P. T., Dickson, D. W., Trojanowski, J. Q., Jack, C. R., Boyle, P. A., Arfanakis, K., Rademakers, R., Alafuzoff, I., Attems, J., Brayne, C., Coyle-Gilchrist, I. T. S., Chui, H. C., Fardo, D. W., Flanagan, M. E., Halliday, G., Hokkanen, S. R. K., Hunter, S., Jicha, G. A., Katsumata, Y., … Schneider, J. A. (2019). Limbic-predominant age-related TDP-43 encephalopathy (LATE): Consensus working group report. Brain: A Journal of Neurology, 142(6), 1503–1527. https://doi.org/10.1093/brain/awz099 Oh, J., Eser, R. A., Ehrenberg, A. J., Morales, D., Petersen, C., Kudlacek, J., Dunlop, S. R., Theofilas, P., Resende, E. D. P. F., Cosme, C., Alho, E. J. L., Spina, S., Walsh, C. M., Miller, B. L., Seeley, W. W., Bittencourt, J. C., Neylan, T. C., Heinsen, H., &Grinberg, L. T. (2019). Profound degeneration of wake-promoting neurons in Alzheimer’s disease. Alzheimer’s & Dementia, 15(10), 1253–1263. https://doi.org/10.1016/j.jalz.2019.06.3916 Signaevsky, M., Prastawa, M., Farrell, K., Tabish, N., Baldwin, E., Han, N., Iida, M. A., Koll, J., Bryce, C., Purohit, D., Haroutunian, V., McKee, A. C., Stein, T. D., White, C. L., Walker, J., Richardson, T. E., Hanson, R., Donovan, M. J., Cordon-Cardo, C., … Crary, J. F. (2019). Artificial intelligence in neuropathology: Deep learning-based assessment of tauopathy. Laboratory Investigation; a Journal of Technical Methods and Pathology, 99(7), 1019–1029. https://doi.org/10.1038/s41374-019-0202-4 Ståhl, P. L., Salmén, F., Vickovic, S., Lundmark, A., Navarro, J. F., Magnusson, J., Giacomello, S., Asp, M., Westholm, J. O., Huss, M., Mollbrink, A., Linnarsson, S., Codeluppi, S., Borg, Å., Pontén, F., Costea, P. I., Sahlén, P., Mulder, J., Bergmann, O., … Frisén, J. (2016). Visualization and analysis of gene expression in tissue sections by spatial transcriptomics. Science, 353(6294), 78–82. https://doi.org/10.1126/science.aaf2403 Tang, Z., Chuang, K. V., DeCarli, C., Jin, L.-W., Beckett, L., Keiser, M. J., &Dugger, B. N. (2019). Interpretable classification of Alzheimer’s disease pathologies with a convolutional neural network pipeline. Nature Communications, 10(1), 2173. https://doi.org/10.1038/s41467-019-10212-1 Uemura, N., Yagi, H., Uemura, M. T., Hatanaka, Y., Yamakado, H., & Takahashi, R. (2018). Inoculation of α-synuclein preformed fibrils into the mouse gastrointestinal tract induces Lewy body-like aggregates in the brainstem via the vagus nerve. Molecular Neurodegeneration, 13(1), 21. https://doi.org/10.1186/s13024-018-0257-5 Zamanian, J. L., Xu, L., Foo, L. C., Nouri, N., Zhou, L., Giffard, R. G., & Barres, B. A. (2012). Genomic analysis of reactive astrogliosis. The Journal of Neuroscience: The Official Journal of the Society for Neuroscience, 32(18), 6391–6410. https://doi.org/10.1523/JNEUROSCI.6221-11.2012 Copyright: © 2020 The author(s). This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited, a link to the Creative Commons license is provided, and any changes are indicated. The Creative Commons Public Domain Dedication waiver (https://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. |