Research Article
Moral Distress Among Consumer Health Information
Professionals: An Exploratory Study
Robin O'Hanlon
Associate Librarian, User
Services
Memorial Sloan Kettering
Cancer Center Library
New York, New York, United
States of America
Email: ohanlonr@mskcc.org
Katelyn Angell
Associate
Professor/Coordinator of Library Instruction
Long Island University,
Brooklyn Campus Library
Brooklyn, New York, United
States of America
Email: Katelyn.Angell@liu.edu
Samantha Walsh
Manager of Information &
Education Services
Levy Library
Icahn School of Medicine at
Mount Sinai
New York, New York, United
States of America
Email: Samantha.walsh@mssm.edu
Received: 10 Oct. 2020 Accepted: 5 Apr. 2021
![]() 2021 O’Hanlon, Angell, and Walsh. This
is an Open Access article distributed under the terms of the Creative Commons‐Attribution‐Noncommercial‐Share Alike License 4.0
International (http://creativecommons.org/licenses/by-nc-sa/4.0/),
which permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly attributed, not used for commercial
purposes, and, if transformed, the resulting work is redistributed under the
same or similar license to this one.
2021 O’Hanlon, Angell, and Walsh. This
is an Open Access article distributed under the terms of the Creative Commons‐Attribution‐Noncommercial‐Share Alike License 4.0
International (http://creativecommons.org/licenses/by-nc-sa/4.0/),
which permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly attributed, not used for commercial
purposes, and, if transformed, the resulting work is redistributed under the
same or similar license to this one.
Data Availability: O'Hanlon,
R., Angell, K., Walsh, S. (2021). Raw dataset and interview codebook for
"Moral Distress Among Consumer Health Information Professionals: An
Exploratory Study"[Dataset]. Edmonton, Canada: UAL Dataverse.
Retrieved from https://doi.org/10.7939/DVN/LZHZHC
DOI: 10.18438/eblip29871
Abstract
Objectives – In recent
years, moral distress has become a topic of interest among health
professionals. Moral distress is most commonly described in the nursing
literature, and refers to a situation wherein an individual knows the correct
action to take, but is constrained from doing so. While moral distress differs
from the classic ethical dilemma, in recent years practitioners and theorists
have advocated for a broadening of the definition of moral distress. To date,
no study has examined another group of individuals who frequently interact with
patients and who may be constrained by the confines of their role - Consumer
Health Information Professionals (CHIPS). The objective of this study was to
determine if CHIPS experience moral distress and/or ethical dilemmas, and to
determine what, if any, coping strategies these individuals have developed.
Methods – This study employed a mixed methods approach.
Quantitative data were gathered via an online survey which was distributed to
relevant consumer health information professional electronic mail lists. The
survey contained demographic questions and a series of questions related to
potential discomfort within the context of work as a consumer health
information professional. Qualitative data were also gathered through phone
interviews with CHIPS. Interview questions included the participant’s
definition of moral distress, professional experiences with moral distress, and
any coping strategies to manage said distress.
Results – The authors
received 213 survey responses. To test whether any of our demographic variables
help to explain survey response, we used STATA to calculate Pearson correlation
coefficients. Individuals who were more likely to experience discomfort in
their occupation as CHIPS included individuals with less experience and
individuals who identified as Black and Latinx. Interview data indicated that
participants most commonly experienced ethical dilemmas related to censorship,
providing prognosis information, and feeling constrained by institutional policies.
Few interview participants described scenarios that reflected moral distress.
Conclusions – CHIPS do
not appear to experience moral distress, at least according to its most narrow
definition. CHIPS do consistently experience distinct ethical dilemmas, and the
most durable patterns of this phenomenon appear to be related to experience
level and racial identity. In recent years, researchers have raised calls to
broaden the definition of moral distress from its narrow focus on constraint to
include uncertainty, and CHIPs do experience moral uncertainty in their work.
Further study is needed to determine how to best address the impacts of
discomfort caused by ethical dilemmas among these groups.
Introduction
Originally discussed in nursing literature, the concept
of moral distress is evolving and has more recently been explored in various
healthcare professions. In 1984, Andrew Jameton
described moral distress as a phenomenon that arises “when one knows the right
thing to do, but institutional constraints make it nearly impossible to pursue
the right course of action” (Jameton, 1984, p. 6).
While Jameton and his contemporaries’ discourse
focused on the experiences of nurses, researchers have become interested in
exploring this concept outside of the nursing profession, as well as beyond
situations involving an institutional constraint. Fourie (2015) sought to
expand the definition of moral distress beyond nurses and experiences of
constraint, proposing that moral distress occurs when health professionals
experience a psychological response due to a moral conflict, restraint, or
uncertainty.
While
this evolved definition allows us to explore the experiences of all healthcare
workers, it is important to understand the difference between moral distress,
moral conflict, and ethical dilemmas. Moral conflict occurs when “when duties
and obligations of healthcare providers or general guiding ethical principles
are unclear” (Jormsri, 2004, p. 217), while an
ethical dilemma involves “the need to choose from among two or more morally
acceptable options or between equally unacceptable courses of action, when one
choice prevents selection of the other” (Ong et al., 2012, p. 11). Ethical
dilemmas and moral conflicts are often closely related to the experience of
moral distress in healthcare professionals. As these concepts are explored and
refined, the authors of this study sought to understand the experience of
Consumer Health Information Professionals (CHIPS). CHIPS are information
professionals providing consumer health information, or health information to
non-healthcare professionals, in a variety of settings (Reference and User
Services Association, 2015). Working in public, hospital, and other specialized
libraries, these professionals regularly interact with patients and families at
distressing times. While there is a growing interest in moral and ethical
issues within the Library and Information Sciences profession, information
professionals who provide healthcare information to the public have not been
the focus of a study on moral distress. These information professionals
frequently interact with patients in a variety of settings, and may be
constrained by their role, resources, or institution. Furthermore, one author personally
experienced a feeling of constraint while assisting a patron with a consumer
health information inquiry.
Literature
Review
Beginning
in the 1980’s, the majority of studies exploring moral distress consider the
experiences of nurses. This continued focus is because Jameton’s
formative definition of moral distress necessitates the existence of
“institutional constraints” (1984, p. 6). Many researchers describe nurses as
particularly prone to situations where they must carry out and often bear the consequences
of others’ decisions (Marshall & Epstein, 2016). Similarly, the Moral
Distress Scale, developed by Corley (1995), which measures nurses’ experiences
of moral distress, focuses on various limitations of agency, such as
“institutional constraint.” Exploring nurses’ experiences using the Moral
Distress Scale as well as other measures, researchers have found that moral
distress manifests in various forms of psychological distress as well as
physical manifestations. In a recent review, Morley, Ives, and Bradbury-Jones
(2019) report “sleeplessness, nausea, migraines, gastrointestinal upset,
tearfulness and physical exhaustion” (p. 655) in nurses experiencing moral
distress. This phenomenon also has a direct effect on patient care, as Oh and Gastmans’ (2015) report that nurses with a high level of
moral distress experience depersonalization, where they emotionally distance
themselves from patients. Finally, moral distress is a documented threat to the
healthcare workforce itself, as Whitehead, Herbertson,
Hamric, Epstein, and Fisher (2015) reported that “providers who had left or
considered leaving a position in the past reported moral distress mean levels
significantly higher than those who had never considered leaving” (p. 123). It
is important to note that Whitehead et al.’s survey included all healthcare
professionals in the authors’ healthcare system.
In
recent years, researchers have studied moral distress in non-nursing healthcare
professions, such as healthcare assistants (Rodger, Blackshaw,
& Young, 2019), veterinarians (Moses, Malowney,
& Wesley Boyd, 2018), medical students (Camp & Sadler, 2019), physician
trainees and residents (Dzeng et al., 2015; Sajjadi, Norena, Wong, & Dodek, 2016), and Oncologists (Hlubocky,
Spence, McGinnis, Taylor, & Kamal, 2020). This research is happening in
tandem with the evolution of Jameton’s formative
definition, as evidence of moral distress is becoming apparent across
healthcare fields. Like many nursing researchers, Sajjadi
et al. (2016) also report an increased likelihood to leave the job or
profession in internal medicine residents experiencing high levels of moral
distress. While we are beginning to appreciate the prevalence of moral distress
among a variety of patient-facing healthcare workers, studies have not focused
on the experiences of CHIPS.
At
the time of this writing, Library and Information Science (LIS) literature has
reported very little research on moral distress and moral conflict. Most
research on the broader topic of the distinction between right and wrong within
matters relating to the profession has focused primarily on ethical dilemmas.
Despite the fact that research nearly 30 years ago explored “moral conflict” as
experienced by librarians, recent scholarship has not expanded upon this topic
much. This is particularly surprising within health and medical librarianship,
as broader medical literature continues to assess related concepts of morality.
This paper can help contribute to the development of a body of knowledge on
morality within library and consumer health information literature.
In
1993 Broderick describes 19th century librarians as self-defined “moral
arbiters” (p. 447) of society, responsible for determining appropriate and
inappropriate information for their constituencies. Framed in the context of
collection development, the central thesis of the piece is the obligation of
public libraries to shirk the idea of a universal morality and acquire
materials with myriad points of view on a subject. Low (2002) also examines moral
conflicts within collection development, specifically related to the tension
film librarians can face when deciding between acquiring movies featuring a
diverse array of perspectives and dominant preferences of the library’s parent
company. He argues that true morality cannot exist in a library collection
“without recognizing all voices, i.e. without a balance of perspectives” (p.
40).
However,
ethical dilemmas have been repeatedly addressed in various library settings,
including hospital, academic, and public. Librarians experience ethical
quandaries across departments and roles, including reference services (Luo
& Trott, 2016), reader’s advisory (Lawrence, 2020), the organization of
information (McCourry, 2015), privacy/confidentiality
(Elliott, 2015), and RFID technology (Thornley, Ferguson, Weckert,
& Gibb, 2011). Some researchers are generating strategies for preparing
people to resolve ethical dilemmas before they even complete their LIS graduate
programs. Walther (2016) details the development of problem-based learning
techniques to teach LIS graduate students critical skills for handling ethical
dilemmas in their future careers. This pedagogy is framed in part by the
definition of an ethical l dilemma as occurring when “two or more moral
obligations come into conflict” (Walther, p.181).
Murphy
(2001) elucidates ethical dilemmas faced by hospital librarians, chiefly the
pressure to choose between prioritizing the needs of their institution versus
collective social welfare, or the mores of the broader library profession. The
stakes are high here, as the actions of hospital librarians directly impact the
physical and psychological well-being of patrons (patients and their loved
ones). Rigorous training in and dissemination of the professional ethics of the
field can help this disconnect. Professional codes, such as the Medical Library
Association’s Code of Ethics for Health Sciences Librarianship (last updated in
2010), can play an important role in individually or collaboratively working
through job-related ethical dilemmas.
In
2014 Byrd, Devine, and Corcoran surveyed 500 MLA members and learned that while
80% of respondents knew of the Code, nearly one third were unaware when they
last consulted it for guidance. While clearly an invaluable resource for
information professionals, the Code’s principles do not directly address
morality within informed decision making. One participant of this study, when
surveyed on key issues that the Code does not explicitly cover, responded that
“honesty, fairness and morality” (p. 269) should be added as principles that
librarians are professionally obligated to follow.
Aims
The impetus for this study was grounded first and
foremost in a combination of shared professional and close personal connections
with nurses, as well as professional experiences as information professionals.
One author identified a feeling of moral distress caused by constraint in
assisting a patron with a consumer health information inquiry, and began to
construct a project to deeper examine these experiences. All three authors have
encountered ethical dilemmas in the course of either providing consumer health
information services or teaching research skills to nursing students.
Two research questions can be used to frame this study.
First, do CHIPS experience moral distress or ethical dilemmas while performing
their daily job duties? Secondly, if
individuals experience moral distress or ethical dilemmas, what coping
strategies, if any, have they developed?
Methods
The
study employed a mixed methods approach. In April 2020, the study was
determined to meet the regulatory exemption for IRB by Memorial Sloan Kettering
Cancer Center’s Human Research Protection Program under 45 CFT.101(d)(2).
Contemporary
moral distress instruments (e.g., the Moral Distress Scale-Revised) are heavily
focused on issues surrounding direct patient care, which may not be applicable
to CHIPS. As a result, we developed an instrument using the secure web
application REDCap.
The survey contained questions on basic demographic and
occupational questions along with a series of questions designed to measure
feelings of discomfort and distress within the context of consumer health
information librarianship. To assess personal values, the survey also asked
belief-oriented questions related to patient advocacy and empowerment.
Non-demographic questions were posed on a Likert scale from 1-6 (1 = Strongly
Disagree; 2 = Disagree; 3 = Mildly Disagree; 4 = Mildly Agree; 5 = Agree; 6 =
Strongly Agree). The survey instrument has been included as Appendix A. The
survey questions were primarily intended to measure CHIPS’ experiences of
ethical dilemmas. However, because of the somewhat ambiguous nature of
moral/ethical phenomena, some of the survey questions could address both
ethical dilemmas and moral distress, depending on how the respondent
interpreted the question. For example, for question #3
(“I feel licensing agreements with vendors prohibit me from sharing information
with patients in the way I would like”) one could argue that a respondent who
“agrees” or “strongly agrees” with this statement is experiencing moral
distress because he/she/they feels that providing free and unencumbered access
to information for all consumers is the morally correct course of action, and
feels constrained by licensing agreements. This person may, on
moral grounds, feel that all information should be free and that any barriers
to openness are morally reprehensible. However, one could also argue that a
respondent who “agrees” or “strongly agrees” is experiencing an ethical dilemma
if they feel that both choices are morally acceptable and
simply don’t know which to choose. This respondent might respect the legality
of restrictions to proprietary information and feel they have these
restrictions have value, but at the same time may wish their patrons could have
free access.
The survey was disseminated in early May 2020 and
remained open to responses until June 16, 2020. It was disseminated to 22
electronic mail lists geared towards medical, academic, and public library
information professionals. No incentive was offered for completing the survey.
STATA was used to complete statistical analysis. The raw survey data has been
openly deposited.
Survey respondents had the option to include their
contact information if they wished to participate in a follow-up interview.
While the survey assessed if CHIPS were experiencing distress in general, the
aim of the interviews was to determine if the distress CHIPS experience occurs
within the context of moral distress or ethical dilemmas.
Interview questions were open ended and focused on three
components: 1) the participant’s understanding and personal definitions of
moral distress, 2) the participant’s experience with moral distress in the
context of being a consumer health information professional, 3) any coping
strategies the participant had developed to manage moral distress. Interviews
continued until a saturation point in thematic information was reached,
resulting in 14 total interviews. Due to time constraints, only one author
coded the interviews. Interviews were manually coded in a Google sheet,
resulting in 21 codes. Wherever possible, the author used rich or thick
descriptions assessing the interview data, making the code descriptions as
detailed as possible. Appendix B includes the interview schedule. The interview
codebook has been openly deposited with the raw data.
Interviews were conducted by one author using Zoom. Prior
to the interviews, participants received informed consent documentation. Phone
interviews were recorded and transcribed using TapeACall
Pro software. Zoom interviews were recorded and manually transcribed.
Interviews completed by phone were automatically transcribed using the TapeACall Pro transcription feature, but required some
manual cleanup. Interviews took place in May 2020 and June 2020.
Survey Population and Demographics
Consumer health information (CHI) is defined as
“information on health and medical topics provided in response to requests from
the general public, including patients and their families. In addition to
information on the symptoms, diagnosis and treatment of disease, CHI
encompasses information on health promotion, preventive medicine, the determinants
of health and accessing the health care system” (Reference and User Services
Association, 2015). Any professional working in this role and self-identifying
as a CHIP qualified to participate in this study.
The authors received 213 survey responses; Table 1
presents summary statistics of this sample. The majority of the respondents
identified as female (81%); white (62%); had a MLS, MIS, or MLIS degree
(66.2%); or had an MLS, MIS, or MLIS and another advanced degree (16.9%),
bringing the total of respondents who had an MLS, MIS, or MLIS to 83%.
Respondents were aged 41-60 (49%), and were not licensed as medical
professionals (94%). Ten respondents preferred not to provide either racial
identity (3.3%) or gender identity (1.4%) and were excluded from the regression
analyses. Respondents were mainly employed by academic medical centers (43%),
hospitals (28%), and public libraries (16%). The amount of experience among
respondents was fairly evenly distributed, 8-20 years’ experience was most
frequently reported (30%), and over 20 years’ experience the least frequently
reported (21%).
In order to understand how our sample compared to the
overall population, we examined data from a demographic survey of Medical
Library Association members (Pionke, 2019). We found
that compared to the respondents in the MLA survey (n=918), our respondents
identified as being less white (62% vs. 72%), slightly more female (81% vs.
79%), and were similar in age range. It should be noted, however, that only 1%
of the respondents in the MLA study identified “consumer health” as their
primary job function.
Table
1
Sample
Characteristics
|
|
N |
% |
|
Age |
|
|
|
Under
25 |
5 |
2.3% |
|
25-30 |
16 |
7.5% |
|
31-40 |
35 |
16.4% |
|
41-50 |
50 |
23.5% |
|
51-60 |
56 |
26.3% |
|
61-70 |
40 |
18.8% |
|
70+ |
11 |
5.2% |
|
Gender
Identity |
|
|
|
Female |
173 |
81.2% |
|
Male |
33 |
15.5% |
|
Gender
non-binary |
4 |
1.9% |
|
Prefer
not to say |
3 |
1.4% |
|
Racial
Identity |
|
|
|
White/Caucasian |
133 |
62.4% |
|
African
American/Black |
24 |
11.3% |
|
Hispanic/Latinx |
24 |
11.3% |
|
Asian
American/Asian |
12 |
5.6% |
|
American
Indian/Alaska Native |
1 |
0.5% |
|
Native
Hawaiian/Pacific Islander |
0 |
0.0% |
|
Middle
Eastern/North African |
2 |
0.9% |
|
Prefer
not to respond |
7 |
3.3%% |
|
Other/not
provided |
10 |
4.7% |
|
Educational
Background |
|
|
|
Master
of Library and Information Science/Master of Library Studies/Master of
Information Studies |
141 |
66.2% |
|
MLS,
MLIS, or MIS AND other advanced degree (i.e. other master’s degree or
doctoral degree) |
36 |
16.9% |
|
Advanced
degree (i.e. other master’s degree or doctoral degree), not MIS, MLIS, or MLS |
18 |
8.4% |
|
Other |
11 |
5.2% |
|
Undergraduate
degree only |
7 |
3.3% |
|
Medical License |
|
|
|
Does
not have a medical license |
201 |
94.4% |
|
Does
have a medical license |
12 |
5.6% |
|
Years of
Consumer Health Experience |
|
|
|
Less
than 12 months |
8 |
3.8% |
|
1-4
years |
39 |
18.3% |
|
4-8
years |
39 |
18.3% |
|
8
years-15 years |
53 |
24.9% |
|
15
years-20 years |
29 |
13.6% |
|
20
years-25 years |
22 |
10.3% |
|
25
years-over 35 years |
23 |
10.8% |
|
Years in
Current Position |
|
|
|
Less
than 12 months |
12 |
5.6% |
|
1-4
years |
60 |
28.2% |
|
4-8
years |
40 |
18.8% |
|
8
years-15 years |
43 |
20.2% |
|
15
years-20 years |
28 |
13.2% |
|
20
years-25 years |
15 |
7.0% |
|
25
years-over 35 years |
15 |
7.0% |
|
Type of Institution Where Employed |
|
|
|
Private
hospital |
5 |
2.4% |
|
Not-for-profit
hospital |
45 |
21.1% |
|
Community
hospital |
6 |
2.8% |
|
Academic
medical center |
48 |
22.5% |
|
Academic
library |
39 |
18.3% |
|
Community
health center |
0 |
0% |
|
Government
agency |
17 |
8.0% |
|
Public
library |
30 |
14.1% |
|
Unemployed |
1 |
0.47% |
|
Other |
22 |
10.3% |
Results
Table 2 presents average Likert scores (1 = Strongly
Disagree, 6 = Strongly Agree), standard deviations, and overall proportions of
responses for questions relating to moral distress. High average Likert scores
(5+) indicate that the majority of respondents overwhelmingly agreed or
strongly agreed with a particular statement. For example, respondents expressed
strong preferences for patient rights (90.6% agreed or strongly agreed that
patients should have access to as much health information as they wish; 92.9%
agreed/strongly agreed that health professionals should take an active role in
patient education and engagement). Similarly, these variables report small
standard deviations (less than 1), indicating that the distribution of Likert
scale responses is highly bunched.
Conversely, low average Likert scores (less than 3) were
more common on questions which emphasized CHIP unpreparedness. Over half of the
sample disagreed with the statements “I often feel unable to provide patients
with the health information they are looking for” and “I often worry that I
lack the necessary skills, education or knowledge.” However, standard
deviations on these “disagree” statements were larger (1.4 and 1.5,
respectively), indicating more variability in response.
While clear majorities emerged in response to certain
issues, respondents were also divided around numerous issues. A fairly even
split in agreement and disagreement can be seen in response to the question
regarding patients confusing the role of the information professional with the
role of a health care provider and not having enough time to spend with
patients. About a third of respondents said they did not feel pressured to
provide prognosis information to patients, or provide them with positive
information about their prognosis, but respondents were likely to feel that
they often must inform patients that the information resources they have
located on their own were not evidence based.
Similarly, responses related to institutional pressure
were mixed. While almost a quarter of respondents agreed with the statement
that licensing agreements prohibited sharing information with patients, more
than one quarter disagreed with this statement. Even though one third of
respondents did not feel torn between the different constituencies they worked
with, nearly 44% reported feeling frustrated with the many roles they were
expected to perform.
Table
2
Likert Scores
|
Question |
% Strongly Disagree |
% Disagree |
% Mildly Disagree |
% Mildly Agree |
% Agree |
% Strongly Agree |
|
"I often
feel unable to provide patients with the health information they are looking
for." |
16.9% n=36 |
37.6% n=80 |
10.8% n=23 |
17.8% n=38 |
14.6% n=31 |
2.3% n=5 |
|
"I often
worry that I lack the necessary skills, education, or knowledge to provide
patients with the information they are looking for." |
16.9% n=36 |
38% n=81 |
10.8% n=23 |
15% n=32 |
13.1% n=28 |
6.1% n=13 |
|
"I feel
like licensing agreements with vendors prevent me from sharing information
with patients in the way I would like." |
16.0% n=34 |
26.3% n=56 |
8.0% n=17 |
15.5% n=33 |
24.4% n=52 |
9.9% n=21 |
|
"I often
feel like patients confuse my role with their health care provider." |
9.4% n=20 |
27.2% n=58 |
10.3% n=22 |
15.5% n=33 |
29.1% n=62 |
8.5% n=18 |
|
"I often
feel like I do not have adequate time to spend on search requests for
patients." |
10.8% n=23 |
28.2% n=60 |
10.8% n=23 |
14.1% n=30 |
26.3% n=56 |
9.9% n=21 |
|
"I often
feel pressured to provide prognosis information or survival rates for
patients." |
16.4% n=35 |
30% n=64 |
12.2% n=26 |
11.3% n=24 |
24.4% n=52 |
5.6% n=12 |
|
"I often
feel patients expect me to provide them with positive information about their
prognosis." |
8.5% n=18 |
31.0% n=66 |
12.2% n=26 |
17.8% n=38 |
22.1% n=47 |
8.5% n=18 |
|
"I often
feel I must inform patients the resources they have found on their own are
not evidence based, credible or reliable." |
3.8% n=8 |
11.3% n=24 |
6.1% n=13 |
17.8% n=38 |
41.3% n=88 |
19.7% n=42 |
|
“I often feel
torn between the different constituencies (e.g. patients, administrators,
clinicians) with whom I work.” |
7.5% n=16 |
33.3% n=71 |
9.9% n=21 |
16.9% n=36 |
22.5% n=48 |
9.9% n=21 |
|
"I feel
frustrated with the many roles I am expected to perform." |
7% n=15 |
25.4% n=54 |
7.5% n=16 |
16% n=34 |
29.1% n=62 |
15% n=32 |
|
"I often
feel caught in the middle between trying to appease patients, caregivers, and
their own health care providers." |
11.7% n=25 |
17.8% n=38 |
12.2% n=26 |
16.4% n=35 |
33.3% n=71 |
8.5% n=18 |
|
"I am
able to successfully cope with the challenges of my position." |
2.3% n=5 |
11.3% n=24 |
5.6% n=12 |
16.4% n=35 |
54% n=115 |
10.3% n=22 |
|
"My
library has an adequate budget." |
8.9% n=19 |
26.8% n=57 |
8.9% n=19 |
14.1% n=30 |
33.3% n=71 |
8% n=17 |
|
"My
library has adequate staff with expertise in providing consumer health
information services." |
8.4% n=18 |
28.2% n=60 |
10.3% n=22 |
20.2% n=43 |
28.2% n=60 |
4.7% n=10 |
|
"I am
able to acquire the resources I need to meet the information needs of my
users." |
2.3% n=5 |
40.4% n=86 |
9.9% n=21 |
17.8% n=38 |
21.6% n=46 |
8% n=17 |
|
"I have
been concerned for my physical or mental health during times of emergency
(e.g., terrorist attacks, pandemics, natural disasters) at my library." |
8.5% n=18 |
24.4% n=52 |
9.9% n=21 |
22.5% n=48 |
21.6% n=46 |
13.1% n=28 |
|
"The
administration of my organization understands the value and importance of my
library." |
9.4% n=20 |
24.9% n=53 |
6.6% n=14 |
14.1% n=30 |
33.3% n=71 |
11.7% n=25 |
|
"I
believe patients and caregivers should have access to as much health information
as they wish." |
0% n=
0 |
1.9% n=4 |
2.3% n=5 |
5.2% n=11 |
33.8% n=72 |
56.8% n=121 |
|
"I
believe patients and caregivers should be active advocates for their own
health care." |
0% n=
0 |
0% n=
0 |
1.4% n=3 |
5.2% n=11 |
33.3% n=71 |
60.1% n=128 |
|
"I
believe health professionals should take an active role in patient education
and engagement." |
0% n=0 |
0.5% n=1 |
0.5% n=1 |
6.1% n=
13 |
32.9% n=70 |
60.1% n=128 |
Regression Analysis
To test whether any of our demographic variables help to
explain survey response, we used Stata 14 to calculate Pearson chi-squared
tests of independence. Response patterns about patient access and advocacy were
systematically different by racial identity in a statistically significant
manner (χ2=27.4, p=.007 and χ2=18.2, p=.033). Similarly, men tended to disagree
more with the idea that health professionals should take a role in educating
patients, and that they were being asked to provide prognosis information
(χ2=29.8, p=.000 and χ2=23.9, p=.008). Figure 1 displays a spineplot
for the results, by gender, for the question "I often feel pressured to provide prognosis information or
survival rates for patients." Figure 2 presents the question results
by racial identity. Spineplots were created in Stata,
utilizing a software package designed by Cox (2008).
Those who worried about being unprepared were
statistically more likely to be the young (χ2=58.1, p=.000, for the variable
“unprepared,” and χ2=84.1 , p=.000 for the variable “imposter”) and those in
the field for shorter durations ( χ2=25 p=.049 for the variable “unprepared” and χ2=45.7 p=.000 for the variable “imposter”).
We also found that those who identify as Black or Latinx are more likely to
feel frustrated with role confusion when it concerns their jobs as CHIPS ( χ2=54 , p=.000). These racial identity groups also report
that they feel required to provide positive responses to patron inquiries, to
provide prognosis information, and are more likely to fear for their safety
while at work in statistically significant patterns (χ2=84.1 , p=.000, χ2=86.6
, p=.000, and χ2=56.7 , p=.000).
Interview Data Characteristics
Fourteen interviews were conducted and interview
participants were first asked to give their personal definition of moral
distress. Some interviewees gave definitions that closely matched the “classic”
definition of moral distress, but more often their definitions were more
closely aligned with a moral or ethical dilemma. Some interviewees were unable
to provide a clear definition, but instead referred to a survey question that
particularly resonated with them. This resulted in 4 original definitions
provided during the 14 interviews.
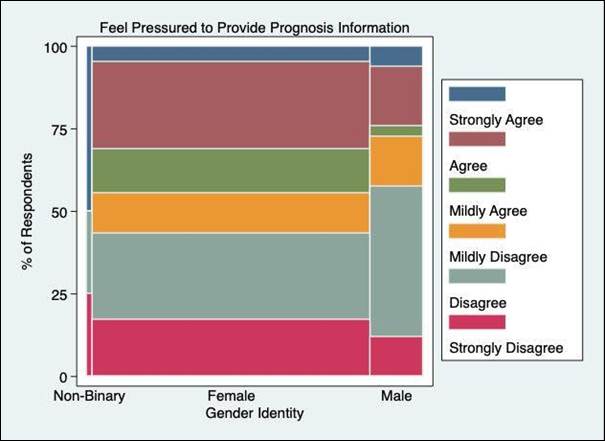
Figure 1
Respondents’ perceptions of providing prognosis
information by gender.

Figure 2
Respondents’ perceptions of
providing prognosis information by racial identity.
The authors asked interview participants to identify how
they experienced moral distress in their work as CHIPS, and several themes
emerged. The first centered around role confusion, wherein consumers do not
understand the purpose of the consumer health library or the role of the
consumer health information professional, and do not recognize that the
consumer health information professional is not a health professional.
Respondents noted that this role confusion usually manifests in patrons seeking
specific medical advice or recommendations from them, including dosing
information for medications or interpreting medical test results.
Several interview participants reported feeling
discomfort when having to inform patients that the information they have found
on their own was not evidence based. In doing their own health information
research, consumers may find health information and then desire “confirmation”
from a consumer health information professional that the information they have
found is in fact evidence based. Respondents report this is more common when
patients are seeking alternative or integrative therapies in place of, rather
than in complement to, traditional medicine. Another common source of internal
conflict among the interview participants related to being asked to provide
prognosis information including survival rates/outcomes:
"I have that
mental list of diagnoses that I want people to not ask me. Because I know what
the situation looks like, pancreatic cancer, for example. I hate it. Especially
in a case like that, when survival rates aren't good, but they don't know that
yet. So they are just looking at treatment situations or whatever. And I never
know how far to go. Like should I be offering them information on palliative
care?”
Several interview participants raised the issue of
providing “too much” information, particularly when assisting patients who were
newly diagnosed with a condition that has particularly dire outcomes.
Participants reported not wanting to “overwhelm” their patrons with information,
but feeling that not providing them with the level of information requested
would amount to censorship:
"I… worry
about inadvertently being a censor, not providing them with enough information
for them to make a health care decision because I know they're not at a place
where they can do that effectively."
A lack of available information on a particular health
topic was also often a source of discomfort for interview participants. In this
instance, assisting individuals with rare diseases and conditions can be
particularly challenging. Other participants reported frustration with being
unable to find health information resources available in languages other than
English.
Interview participants described several instances
wherein they struggled with institutional policies to remain “neutral:”
“The Library can't
recommend one [health care] facility over another, even though I might know
that one facility has a worse record on something. And that I struggle with,
too, so I'm always saying get a second opinion, look at other places. Here are
the statistics."
One interview participant described a scenario wherein
despite being hired as a “community health librarian,” she had been constrained
by the administration of her institution from actively providing services to
the local community and was instead relegated to providing services to a lower
need community that was directly affiliated with her institution (a
university).
While not directly related to ethical constraints or
dilemmas, interview participants reported several scenarios related to their
work as CHIPS that caused them to feel a sense of generalized distress. Two
interview participants felt they lacked the necessary training and skills to
function competently in their positions and that they experienced feeling of
inadequacy and stress. Finally, interview participants reported that simply
being exposed to the stress of patients, caregivers, and family members can be
upsetting, particularly if they have not received adequate training to cope
with these types of stressors:
"They come in
with a diagnosis, and I'll help them, it's not a good diagnosis, and they'll be
upset. You're trying to help them, and they start crying. They're visibly
upset, which makes me upset."
Interview participants identified several coping
strategies for managing their experiences of moral distress, as well as
emotional distress in the professional setting. Six interview participants
reported relying on a network of professionals for additional support when the
patron they were helping was in distress or if the patron asked for
resources/information beyond the scope of the consumer health information
professional’s role. These professionals include social workers, patient
advocates, volunteer services, patient educators, and dieticians. One
respondent noted the benefits of support from health care providers:
"It's good to
have nurse colleagues who can help me process things, and know how to deal with
weird situations, like being pulled into people's medical and legal issues. As
librarians we want to help, so it's helpful because they know where to refer
people for things like living wills."
Participants reported strengthening their professional networks over
time, as they became more familiar with institutional resources and personnel.
Several participants reported that they simply felt less distress as they
gained familiarity with the types of encounters and requests that typically
upset them, and as they became more comfortable with the demands of their role
and their surroundings. Using a disclaimer (either verbally or in a written
form such as a sign) which described the role of the consumer health
information professional and its limitations was also reported.
Working to ensure patients are effective advocates for
their own health was another coping strategy reported by participants. One
subject described alleviating discomfort by encouraging the patients he worked
with who were feeling overwhelmed by their diagnosis to write down specific
questions they have for their health care provider and to practice asking them
aloud. Other participants reported encouraging patients to bring research
studies or consumer health information they had located to their health care
provider. Other coping strategies were less frequently reported and included
indulging in escapist entertainment, using reflective practice (e.g.,
journaling), using institutional staff assistance programs, and actively
circumventing bureaucratic systems to aid their patrons.
Discussion
The study finds that CHIPS do experience generalized
distress within their professional roles, and in some cases this distress
appears to be directly related to the nature of their role. For example, one
interview participant described her struggle with providing information on
Morgellons Disease, a controversial condition which many health professionals
describe as a form of delusional parasitosis, but has also been described by a
smaller group of medical professionals as a legitimate dermatological
condition. The controversial nature of the condition left this interview
participant feeling torn between her patrons who were convinced they suffered
from the condition and the lack of evidence that the condition actually exists
in the physical sense. CHIPS exist within a sort of interspace, with
significantly more expertise of health information than the average consumer,
but frequently without the licensure, education, and hands on knowledge of
medical professionals. Navigating this interspace may prove challenging,
particularly for individuals who are already faced with navigating
organizational power structures and systemic pathologies (ex., racism, ageism).
Indeed, the distress experienced by consumer health
professionals appears to be related at least in part to the level of support,
or lack thereof, that they receive from their institution at large. While the majority
of respondents felt they were able to successfully cope with the challenges of
their positions (54%), one third reported that their library had an inadequate
budget (33%), inadequate staffing to support consumer health information
services (33%), and that the administration of their organization did not
understand the value and importance of their library (33.3%). About a third
(34.7%) of respondents also reported being concerned for their physical or
mental health during times of an emergency.
While CHIPS appear to experience distress, it is
beneficial to distinguish between distress that occurs in the course of one’s
occupation and distress caused by an ethical
dilemma in a professional context. Again, an ethical dilemma is a situation
in which two moral principles conflict with one another. Not all the scenarios
described by the interview participants were true ethical dilemmas, but some
were, including concerns about censorship, providing prognosis information, and
feeling constrained by institutional policies. The latter phenomenon, a feeling
of institutional constraint, is associated with moral distress, but our
interview participants were more likely to experience scenarios with competing
moral drawbacks, rather than one obvious morally superior option. The most
durable patterns of these experiences of ethical dilemmas appear to be related
to experience level and racial identity.
CHIPS do not appear, though, to experience moral
distress, at least according to its narrow definition (knowing the correct
action to take, but being constrained from doing so by external forces). Why
don’t CHIPS experience moral distress? One reason may be that the key component
of moral distress, as traditionally defined, of “constraint” is less likely to
be present. It may be that case that the constraint CHIPS experience within the
course of their profession is felt less acutely than frontline medical
professionals, such as nurses, who are directly responsible for the health and
safety of patients. It also appears that CHIPS may confuse moral distress and
ethical dilemmas, or conflate the two.
If moral distress is defined more broadly, as suggested
by Fourie (2015), one could argue that CHIPS do indeed experience a degree of
moral distress. Fourie argues that we should recognize that “constraint is not
a necessary condition of moral distress and that such distress can arise from
morally troubling situations other than those of moral constraint” (p. 580) and
that moral distress should be expanded to include experiences related to moral
uncertainty.
Limitations
The authors acknowledge that the study is limited by
several factors. First, because there was no validated instrument to measure
moral distress and ethical dilemmas among consumer health professionals, we did
not use a validated tool. In future research, a validated tool may aid in
further distinguishing between the nuanced and complex experiences of moral
distress and ethical dilemmas. The purposive sampling technique used
(leveraging electronic mail lists of interest to CHIPS) to identify potential
survey respondents may have resulted in a degree of selection bias. Finally,
only one interviewer coded the interviews. Using two or more coders in future
studies would reduce the potential for bias when identifying interview themes,
as long as proper interrater reliability protocols are implemented.
Further Research
While
this study provides burgeoning insight into the exploration of moral distress
among CHIPS, additional research is needed to validate and expand on these
findings to draw broader conclusions.
First,
it would be valuable for outside researchers to apply the survey instrument
developed by the authors to their own samples. The instrument was used for the
first time in the present study, and did not undergo validity or reliability
calculations. This process would help to ensure the instrument is consistent
across applications, measures what it intends to measure, and that results can
be extrapolated to a broader population.
Next,
the results of the survey indicated that participants who are Black or Latinx
experience greater distress in the CHI profession than people of other racial
identities. These statistics are concerning and need further investigation in
efforts to identify and ameliorate any racism or microaggressions causing this
distress. While there aren’t similar studies within LIS scholarship to compare
these findings Dyo, Kalowes,
and Devries (2016) found that Hispanic nurses reported much higher rates of
moral distress than other ethnic groups, “suggesting that culture and ethnicity
may play a role in the perception and experience of moral distress” (p. 1). A
pertinent solution identified within nursing literature to address this problem
was to begin studying moral distress as experienced by non-Western nurses (Prompahakul & Epstein, 2020), a project that could
easily be replicated with CHIPS or librarians.
Conclusions
This study examined how CHIPS experience moral distress,
ethical dilemmas, and the use of coping strategies for managing the negative
impacts of these phenomena. While the study finds that CHIPS do not appear to
experience moral distress according to its narrow definition focused on
constraint, study results indicate that CHIPS do experience ethical dilemmas in
the course of their work. The most durable patterns of ethical distress
experienced by CHIPS appear to be related to experience level and racial identity,
with younger, Black, and Latinx CHIPS experiencing ethical dilemmas at higher
rates. Further study is needed to determine why there is a statistically
significant relationship between these groups and their experiences with
ethical distress. The interview data further elucidates how CHIPS interpret the
phenomenon of moral distress and how this term is sometimes confused with
ethical dilemmas. This issue could be ameliorated by professional associations
creating a module on integral ethical codes of their area of librarianship and
encouraging libraries to include participation in the module in onboarding for
new hires. Additionally, Library and Information Science graduate programs can
build greater content on morals and professional ethics into their foundational
courses. Finally, while the experiences of the study participants do not fit
the classic definition of moral distress, which is characterized by the
presence of constraint, they do align with a more broadly defined version of
moral distress. This definition, as described by Fourie (2015) allows for the
inclusion of the experience of uncertainty to co-exist with the experience of
constraint in moral contexts.
Acknowledgements
The authors would like to thank all survey respondents
and interview participants. Many thanks to Kendra Godwin for her assistance
with reviewing the survey prior to distribution, and thanks to Tedi Brash, Aman Kaur, Barnaby Nicolas, Robb Mackes, and Shawn Stedinger for
their assistance with survey distribution.
The authors would like to thank Sam Stabler for his
assistance with statistical analysis and creating the spineplots.
Author Contributions
Robin O’Hanlon:
Methodology, Formal analysis, Data curation, Visualization, Writing – original
draft (equal), Writing – review & editing (equal) Katelyn Angell:
Methodology, Writing – original draft (equal), Writing – review & editing
(equal) Samantha Walsh: Methodology, Writing – original draft (equal),
Writing – review & editing (equal)
References
Broderick, D. M. (1993). Moral
conflict and the survival of the public library. American Libraries, 24(5),
447–448. https://www.jstor.org/stable/i25632891
Byrd, G. D., Devine, P. J.,
& Corcoran, K. E. (2014). Health sciences librarians' awareness and
assessment of the Medical Library Association Code of Ethics for Health
Sciences Librarianship: The results of a membership survey. Journal of the Medical Library Association:
JMLA, 102(4), 257–270. https://doi.org/10.3163/1536-5050.102.4.007
Camp, M., & Sadler, J.
(2019). Moral distress in medical student reflective writing. AJOBEmpirical Bioethics, 10(1), 70–78. https://doi.org/10.1080/23294515.2019.1570385
Corley, M.C. (1995). Moral
distress of critical care nurses. American
Journal of Critical Care, 4(4),
280–285. https://doi.org/10.4037/ajcc1995.4.4.280
Cox, N. J. (2008). Speaking
Stata: Spineplots and their kin. The Stata Journal, 8(1),
105-121. https://doi.org/10.1177/1536867X0800800107
Dyo, M., Kalowes, P., &
Devries, J. (2016). Moral distress and intention to leave: A comparison of
adult and paediatric nurses by hospital setting. Intensive & Critical Care Nursing, 36,
42-48. https://doi.org/10.1016/j.iccn.2016.04.003
Dzeng, E., Colaianni, A., Roland,
M., Levine, D., Kelly, M., Barclay, S., & Smith, T. (2015). Moral distress
amongst American physician trainees regarding futile treatments at the end of
life: A qualitative study. Journal of
General Internal Medicine, 31(1),
93-99. https://doi.org/10.1007/s11606-015-3505-1
Elliott, K. (2015). Planning
for barriers in hospital library social media implementation. Journal of Hospital Librarianship, 15(1), 13–22. https://doi.org/10.1080/15323269.2015.982013
Fourie, C. (2015). Moral
distress and moral conflict in clinical ethics. Bioethics, 29(2), 91–97. https://doi.org/10.1111/bioe.12064
Hlubocky, F. J.,
Spence, R., McGinnis, M., Taylor, L., & Kamal, A. H. (2020). Burnout and
moral distress in oncology: Taking a deliberate ethical step forward to
optimize oncologist well-being. JCO
Oncology Practice, 16(4),
185–186. https://doi.org/10.1200/OP.20.00030
Jameton, A.
(1984). Nursing practice: The ethical
issues. Prentice Hall.
Jormsri, P.
(2004). Moral conflict and collaborative mode as moral conflict resolution in
health Care. Nursing & Health
Sciences, 6(3), 217-221. https://doi.org/10.1111/j.1442-2018.2004.00191.x
Lawrence, E. E. (2020). On the
problem of oppressive tastes in the public library. Journal of Documentation, 76(5),
1091–1107. https://doi.org/10.1108/JD-01-2020-0002
Low, D. (2002). Moral conflict
for the film librarian. Journal of
Information Ethics, 11(2), 33-45.
https://ir.uwf.edu/islandora/object/uwf:23834
Luo, L., & Trott, B.
(2016). Ethical issues in reference: An in-depth view from the librarians’
perspective. Reference & User
Services Quarterly, 55(3),
189–198. https://doi.org/10.5860/rusq.55n3.188
Marshall, M. F., & Epstein,
E. G. (2016). Moral hazard and moral distress: A marriage made in purgatory. The American Journal of Bioethics: AJOB,
16(7), 46–48. https://doi.org/10.1080/15265161.2016.1181895
McCourry, M. W. (2015). Domain analytic, and domain
analytic-like, studies of catalog needs: Addressing the ethical dilemma of
catalog codes developed with inadequate knowledge of user needs. Knowledge Organization, 42(5), 339–345. https://doi.org/10.5771/0943-7444-2015-5-339
Medical Library Association
(2010). Code of ethics for health
sciences librarianship. https://www.mlanet.org/page/code-of-ethics
Morley, G., Ives, J., Bradbury-Jones, C.,
& Irvine, F. (2019). What is ‘moral distress’? A narrative synthesis of the
literature. Nursing Ethics, 26(3), 646–662. https://doi.org/10.1177/0969733017724354
Moses, L., Malowney,
M. J., & Wesley Boyd, J. (2018). Ethical conflict and moral distress in
veterinary practice: A survey of North American veterinarians. Journal of Veterinary Internal Medicine,
32(6), 2115–2122. https://doi.org/10.1111/jvim.15315
Murphy, S.A. (2001). The
conflict between professional ethics and the ethics of the institution. Journal of Hospital Librarianship, 1(4),
17-30. https://doi.org/10.1300/J186v01n04_02
Oh, Y., & Gastmans, C. (2015). Moral distress experienced by nurses:
A quantitative literature review. Nursing
Ethics, 22(1), 15–31. https://doi.org/10.1177/0969733013502803
Ong, W. Y., Yee, C. M., &
Lee, A. (2012). Ethical dilemmas in the care of cancer patients near the end of
life. Singapore Medical Journal, 53(1), 11–16. https://pubmed.ncbi.nlm.nih.gov/22252176/
Pionke, JJ. (2019). Medical Library Association Diversity and
Inclusion Task Force 2019 survey report. Journal
of the Medical Library Association, 108(3), 503–512. https://doi.org/10.5195/jmla.2020.948
Prompahakul, C., & Epstein, E. G. (2020). Moral distress
experienced by non-Western nurses: An integrative review. Nursing Ethics, 27(3),
778–795. https://doi.org/10.1177/0969733019880241
Reference and User Services
Association (2015). Health and medical
reference guidelines. http://www.ala.org/rusa/resources/guidelines/guidelinesmedical
Rodger, D., Blackshaw,
B., & Young, A. (2019). Moral distress in healthcare assistants: A
discussion with recommendations. Nursing
Ethics, 26(7–8), 2306–2313. https://doi.org/10.1177/0969733018791339
Sajjadi, S., Norena, M., Wong, H.,
& Dodek, P. (2017). Moral distress and burnout in
internal medicine residents. Canadian Medical
Education Journal, 8(1), e36–e43.
https://pubmed.ncbi.nlm.nih.gov/28344714/
Thornley, C., Ferguson, S., Weckert, J., & Gibb, F. (2011). Do RFIDs (radio
frequency identifier devices) provide new ethical dilemmas for librarians and
information professionals? International
Journal of Information Management, 31(6),
546–555. https://doi.org/10.1016/j.ijinfomgt.2011.02.006
Walther, J. H. (2016). Teaching
ethical dilemmas in LIS coursework: An adaptation on case methodology usage for
pedagogy. The Bottom Line, 29(3),
180-190. https://doi.org/10.1108/BL-05-2016-0020
Whitehead, P.
B., Herbertson, R. K., Hamric, A. B., Epstein, E. G.,
& Fisher, J. M. (2015). Moral distress among healthcare professionals:
Report of an institution-wide survey. Journal
of Nursing Scholarship: An Official Publication of Sigma Theta Tau
International Honor Society of Nursing, 47(2),
117–125. https://doi.org/10.1111/jnu.12115
Appendix
A
Survey
Instrument
How
old are you?
Under
25
25-30
31-40
41-50
51-60
61-70
Over
70
What
is your gender?
Female
Male
Gender
non-binary
Prefer
not to say
Which
of these best describes your racial identity?
African
American/Black
American
Indian/Alaska Native
Asian
American/Asian
Native
Hawaiian/Pacific Islander
Hispanic/Latinx
Middle
Eastern/North African
White/Caucasian
Other/Not
Provided
Prefer not to respond
What
is your educational background?
Master
of Information Science
Master
of Library and Information Science
Master
of Library Science
Advanced
degree (i.e., other masters degree or
doctoral
degree), not MIS, MLIS, or MLS
MLS,
MLIS, or MIS AND other advanced degree
(i.e.,
other masters degree or doctoral degree)
Undergraduate
degree only
Other
If
"Other," please describe.
Are
you currently, or have you ever been, a licensed medical professional (e.g.
Registered Nurse, Medical Doctor)?
Yes
No
If
you are currently or have been licensed medical professional in the past,
please describe:
Years
of consumer health librarian experience/providing health information to the
public:
Less
than 12 months
1
year - 2 years
2
years - 4 years
4
years - 6 years
6
years - 8 years
8
years - 10 years
10
years - 12 years
12
years - 15 years
15
years - 20 years
20
years - 25 years
25
years - 35 years
Over
35 years
Years
in current position:
Less
than 12 months
1
year - 2 years
2
years - 4 years
4
years - 6 years
6
years - 8 years
8
years - 10 years
10
years - 12 years
12 years
- 15 years
15
years - 20 years
20
years - 25 years
25
years - 35 years
Over
35 years
Type
of institution where you are employed:
Private
hospital
Not-for-profit
hospital
Community
hospital
Academic
medical center
Academic
library
Community
health center
Government
agency
Public
library
Unemployed
Other
If
"Other," please describe.
For the remaining questions, please select one of the following values that
best describes how
you
feel about each statement below:
Strongly
Disagree
Disagree
Mildly
Disagree
Mildly
Agree
Agree
Strongly
Agree
1)
I
often feel unable to provide patients with the health information they are
looking for.
2)
I
often worry that I lack the necessary skills, education, or knowledge to
provide patients with the information they are looking for.
3)
I
feel licensing agreements with vendors prohibit me from sharing information
with patients in the way I would like.
4)
I
often feel that patients confuse my role with their health care provider.
5)
I
often feel I do not have adequate time to spend on search requests for
patients.
6)
I
often feel pressured to provide prognosis information or survival rates for
patients.
7)
I
often feel patients expect me to provide them with positive information about
their prognosis.
8)
I
often feel I must inform patients the resources they are have found on their
own are not evidence
based,
credible, or reliable.
9)
I
often feel torn between the different constituencies (e.g. patients,
administrators,
clinicians)
with whom I work.
10)
I
feel frustrated with the many roles I am expected to perform.
11)
I
often feel caught in the middle between trying to appease patients, caregivers,
and their health care
providers.
12)
I
am able to successfully cope with the challenges of my position.
13)
My
library has an adequate budget.
14)
My
library has adequate staff with expertise in providing consumer health
information services.
15)
I
am able to acquire the resources I need to meet the information needs of my
users.
16)
I
have been concerned for my physical or mental health during times of emergency
(e.g. terrorist
attacks,
pandemics, natural disasters) at my library.
17)
The
administration of my organization understands the value and importance of my
library.
18)
I
believe patients and caregivers should have access to as much health
information as they wish.
19)
I
believe patients and caregivers should be active advocates for their own health
care.
20)
I
believe health professionals should take an active role in patient education
and engagement.
Contact
information (Optional)
If
you are willing to participate in a phone interview about moral distress and
consumer health librarianship, please include your contact information (name
and email address). Any information professional who provides health
information to the public can participate. If you decide to participate in a
phone interview, your
information
will by anonymous in the final publication.
Please
ONLY include your contact information if you are interested in participating in
a phone interview. If you are not interested in participating in a phone
interview, leave this section blank.
Appendix B
Interview Schedule
- Can you define “moral distress”?
- a) Do you feel you have ever experienced
moral distress in your role as a consumer health librarian (or as an
information professional who provides health information to the public)?
b)
If yes, in what ways have you experienced moral distress in your role as a
consumer health librarian (or as an information professional who provides
health information to the public)?
c)
If yes, how has your experience of moral distress affected your ability to
function in your job and your attitude toward your job?
- a) If you have experienced moral distress
in the course of your profession, what factors have contributed to your
distress (e.g., number of years of experience, type of patient)?
b)
If you have not experienced moral distress in your profession, how do you feel
you have avoided this phenomenon?
- a) If you have experienced moral distress
in the course of your profession, have you employed to lessen your
experience of moral distress?
b)
If you have employed coping strategies, which strategies did you find the most
effective
and why?