Research Article
Information Services in Evidence Based Medical Education: A Review of Implementation Trends
Sedigheh Khani
Ph.D. Candidate in Medical
Librarianship and Information Sciences
School of Health Management
and Information Sciences
Iran University of Medical
Sciences
Tehran, Iran
Email: khani.se@iums.ac.ir; khani.sedigheh@gmail.com
Sirous Panahi
Associate Professor
Department of Medical
Library and Information Science
School of Health Management
and Information Sciences
Iran University of Medical
Sciences
Tehran, Iran
Email: panahi.s@iums.ac.ir
Ali Pirsalehi
Assistant Professor of
Internal Medicine
Clinical Development
Research Center of Taleghani Hospital
Medical School
Shahid Beheshti Medical
University
Tehran, Iran
Email: pirsalehi@sbmu.ac.ir
Ata Pourabbasi
Assistant Professor
Endocrinology and Metabolism
Clinical Sciences Institute
Tehran University of Medical
Sciences
Tehran, Iran
Email: Atapoura@tums.ac.ir
Received: 7 Oct. 2021 Accepted: 26 Apr. 2021
![]() 2021 Khani, Panahi, Pirsalehi,
and Pourabbasi. This is an Open
Access article distributed under the terms of the Creative Commons‐Attribution‐Noncommercial‐Share Alike License 4.0
International (http://creativecommons.org/licenses/by-nc-sa/4.0/),
which permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly attributed, not used for commercial
purposes, and, if transformed, the resulting work is redistributed under the
same or similar license to this one.
2021 Khani, Panahi, Pirsalehi,
and Pourabbasi. This is an Open
Access article distributed under the terms of the Creative Commons‐Attribution‐Noncommercial‐Share Alike License 4.0
International (http://creativecommons.org/licenses/by-nc-sa/4.0/),
which permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly attributed, not used for commercial
purposes, and, if transformed, the resulting work is redistributed under the
same or similar license to this one.
DOI: 10.18438/eblip29860
Abstract
Objective – Evidence based
medical education requires supportive information services to facilitate access
to the needed educational evidence. Information services designed specifically
for evidence based medical education are limited or locally developed for
educational units. For librarians to have an opportunity to cooperate
efficiently with medical educators in evidence based medical education, they
require an empirical prototype for transmission of clinical evidence at the
right place and the right time. Therefore, there is a need to recognize types
of information services which support evidence based medical education. The
purpose of this review is to identify implementation trends of evidence based
educational information services.
Methods – We found
related studies by implementing search strategies in PubMed, EMBASE, Web of
Science, Scopus, LISTA, and Google Scholar with keywords like: evidence based
medical education, information services, and library services. We used
reference-checking and citation-checking of related articles for completing the
process of locating relevant articles. After employing inclusion and exclusion
criteria, we selected 11 articles for inclusion in the review and analyzed them
using a narrative review technique.
Results – After
analyzing the results of the included studies, we identified two elements
categorized as program development and five elements categorized as
implementation trend. Prerequisites of program and the process of designing
were essential parts of program development of information services. Schedule
and type of access, how to receive educational-clinical questions, information
services types, responding time, and providing evidence based
outputs were the elements of the implementation process of educational
supported information services.
Conclusion – Designing an evidence based
educational information service strongly depends on the information needs of
learners at each educational level. Schedule and type of access to information
service, time of responding to the received query, and preparation of evidence
based output are essential factors in designing practical educational-developed
information services.
Introduction
In
the 1990s, David Sackett introduced the concept of evidence based medicine
(EBM). EBM was defined as the use of up-to-date, best evidence in clinical
decision making for a better understanding of causation and prognosis of
disease, and selecting more appropriate diagnostic tests and treatment
strategies based on patient preferences and the clinical condition of the
patient (Sackett et al., 1996). In the practice of EBM, clinicians complement
their clinical expertise with the best available evidence (Sackett et al.,
1996), which evidence is available from systematic clinical research like
systematic reviews, cohort studies, and randomized control trials (Burns et
al., 2011).
EBM
and its applications in different functions of medicine have empowered the medical
community (Djulbegovic
& Guyatt, 2017; Sur & Dahm, 2011). Medical
practice, healthcare management, clinical research, and of course, medical
education has been affected by EBM principles (Djulbegovic
& Guyatt, 2017; Shortell et al., 2007). Evidence Based
Education/Best Evidence in Medical Education (EBE/BEME) makes an effort to
utilize evidence in education (Davies, 1999) and reshape the practices and
approaches of learner training based on the best available evidence (Harden et al.,
2000; Hart & Harden, 2000). The goal of
EBM in clinical practice is to enhance patient treatment, but in medical
education, educators train learners in the practice of EBM to empower them to
use evidence in clinical practice (Guyatt et al.,
1992).
Medical
educators try to have an updated and evidence based approach to their teaching
practice in processes such as curriculum revision or implementing new
instructional techniques (Poirier &
Behnen, 2014). In the
evidence based paradigm of teaching, educators combine up-to-date, quality
evidence with previous experience and current educational approaches (Chessare, 1996). Typical tasks required for
evidence based practice in medical education include phrasing a question,
designing a search strategy, appraising the evidence, and making the required
intervention in the teaching approaches (Davies, 1999; Harden
et al., 2000; Hart & Harden, 2000). A primary
challenge of the above procedure is searching the published literature (Poirier &
Behnen, 2014).
Finding
the best evidence is one of the main challenges of EBE/BEME for medical
educators; often they need assistance to effectively find required evidence (Chessare, 1996;
Harden et al., 2000; Reed et al., 2005). Difficulty in
accessing the empirical educational knowledge has a multidimensional nature.
Medical instructors have expressed some barriers to implementing evidentiary
information in education. Lack of time for finding evidence based knowledge,
the volume of research evidence, lack of educational evidence, lack of access
to evidence based educational databases, and difficulty in finding educational
evidence were found to be obstacles for accessing relevant evidence (Emami et al.,
2019; Onyura et al., 2015; Sandars & Patel, 2015; Suttle et al., 2015; Thomas
et al., 2019). Searching for
evidence consists of two core challenges: how to search for evidence and where
to search for evidence (Haig &
Dozier, 2003a, 2003b).
Information
services fulfill the need for access to evidence in medical practice. The main
purpose of information services in a health system is to enhance the
decision-making of clinicians in the treatment of patients. The actors of an
information service are skilled librarians, and the core activity of
information services is transforming requests for evidence into relevant,
evidence based information which then impacts clinical decision making (Fennessy, 2001). In the process of evidence
based decision making, information services with different implementation
trends were developed to supply qualified and up-to-date evidence for
healthcare practice.
Jordan
and Porritt (2004) established an information service to provide evidence based
information for clinicians and patients. The information service supported both
access to evidence and education for how to utilize what they could access.
MCMASTER+ was another type of evidence based information service, which
organized information based on evidence hierarchy and facilitated finding
required evidence to address related clinical questions (Holland &
Haynes, 2005). McGowan et al.
(2010) developed an information service to provide evidence for primary care
practitioners and enhance clinical decision making. These information services
to support clinical practice had commonalities in their implementation
processes. For example, the process of developing reference services for
clinicians consisted of two main components: first, selecting and adapting
appropriate technology, and second, training the librarian to deliver the
information service. Most of the information services supporting clinical
decision making were developed on the web with a well-defined, user-friendly
interface that enhanced physician access to the best evidence (Holland &
Haynes, 2005; Jordan & Porritt, 2004; McGowan et al., 2010). The process of
delivering needed evidence began from searching, appraising, and summarizing
evidence to transferring it into
practice (Davies et al.,
2017; Holland & Haynes, 2005; Jordan & Porritt, 2004; McGowan et al.,
2010), and reviewing
and updating collected evidence periodically (Jordan &
Porritt, 2004).
Aims
All
of the above evidence based information services were
established for clinical practice, but providing evidence for medical education
needs its own educational-developed information services (Emami et al.,
2019; Onyura et al., 2015). Onyura et al. (2015) stated that the delivery approaches
for evidence based knowledge currently available were insufficient and there
was a need for new approaches for delivering synthesized evidence that have a
concise presentation and are accessible at the point-of-need. In this respect,
identifying the implementation trends of information services designed for
evidence based education can be prototypical for designing evidence based
information services for medical education.
Based
on the hierarchy of information services in the Library, Information Science
& Technology Abstracts (LISTA) database thesaurus (EBSCO, n.d.-a),
information services are developed to fulfill information needs in various
fields such as business, agriculture, community, education, and more. In the
LISTA thesaurus, “information services in education” was defined as the “use of
data storage, organization, search, retrieval, and transmission services in
education” (EBSCO, n.d.-b). In the current study, we identified search,
retrieval, and transmission aspects of information services in education.
Therefore, the aim of this review was to identify the types of information
services that were provided for EBE/BEME and compare the trends of supplying
evidence for supporting student teaching and learners training under the
concept of Evidence Based Educational Information Services (EBEIS).
Methods
Article Selection
We
accessed studies on information services that supported EBE/BEME by searching
databases and performing forward and backward citation tracking of related
articles. We searched PubMed, Embase, Web of Science, Scopus, LISTA, and Google
Scholar using keywords such as “evidence based education,” “evidence based
medical education,” “information service,” and “library service.” Table 1
depicts our search strategy for the PubMed database.
Search Strategy
of PubMed
|
Results |
Search
Strategy |
No. |
|
1,522,557 |
(“Education, medical”[Exp.] OR
teaching[NoExp.] OR education[NoExp.] OR “education, professional”[NoExp.] OR “education, graduate” [NoExp.]
OR “education, continuing” [NoExp.] OR “education,
medical, continuing” [MeSH]) OR (teaching OR
training OR education* OR instruction*) [ti, other
term] |
1 |
|
163,230 |
(“Evidence-based medicine” [Exp.] OR “evidence-based practice”
[NoExp.] OR Evidence-based emergency medicine--education[MeSH] OR
Evidence-based medicine--education[MeSH: NoExp] OR evidence-based practice--education[MeSH:NoExp]) OR “evidence-based”[ti,
ab, other term] |
2 |
|
161,765 |
(“Information services” [NoExp.] OR
“Information storage and retrieval” [NoExp.] OR librarians
[MeSH] OR “libraries, medical” [NoExp.]
OR “libraries, hospital” [MeSH] OR “library
services” [NoExp.]OR“information
dissemination” [MeSH]) OR (librar*
OR information*)[ti, other term] |
3 |
|
1,421 |
1 AND 2 AND 3 |
4 |
|
1,344 |
Limit to:
English language |
5 |
|
721 |
Limit to:
2010/1/1 and 2020/1/2 |
6 |
Inclusion and Exclusion Criteria
After
implementing search strategies in each database, we excluded non-English
articles, as well as articles focused on evidence based dentistry, nursing, and
pharmacy studies. Because fields like dentistry have unique educational needs
versus medicine, we omitted them from the review. We also excluded study types
such as letters, chapters, book reviews, editorials, conference abstracts, and
viewpoints. We included studies that described an empirical experiment on the
structure and trend of implementing an EBEIS. In this review, it was important
that the information services were not applied in non-educational clinical
settings, nor were proposed templates or opinions. We ended up with 11 articles
published between 2010 and 2020 included in the review. We have described the
process of selecting related studies in Figure 1.

Figure
1
PRISMA
flowchart of study selection (Liberati et al., 2009).
We
compared the bibliographic and introductory data of included studies in Table
2.
Table
2
Introductory
Data of Included Studies
|
Trend of
implementation |
Type of
education |
Setting |
Country |
Year implemented |
Year published |
First author |
|
Searching evidence based information and delivery of documents |
REa |
Morning
report/ rounds/ team conference |
Canada |
2009 |
2011 |
(Aitken et
al., 2011) |
|
Curriculum
architecture-based LibGuides |
UGMEb |
Case-oriented problem solving curriculum |
Canada |
2008-09 |
2011 |
(Neves &
Dooley, 2011) |
|
Learning
package service |
RE |
Morning report |
USA |
2002-10 |
2011 |
(Weaver, 2011) |
|
Consulting,
searching and delivering of information resources |
CPEc |
Morning rounds |
Philippines |
2013 |
2014 |
(Santos & Mariano, 2014) |
|
Searching and
providing evidence for clinical questions |
RE |
Patient rounds |
USA |
2012 |
2014 |
(Yaeger &
Kelly, 2014) |
|
Consult
searching service |
RE |
EBM conference |
USA |
2013-15 |
2015 |
(Zeblisky et al., 2015) |
|
Consulting and
delivery searching service |
CEd |
Patient-family
centered rounds |
USA |
2014-15 |
2017 |
(Herrmann et
al., 2017) |
|
Information
service supporting patient-based scenarios designing/ consulting searching
service |
UGME |
Simulated
patient scenarios |
USA |
2017 |
2018 |
(Blake et al.,
2018) |
|
Consult and
delivery information service |
CE |
Inpatient
rounds |
USA |
2016 |
2018 |
(Brian et al.,
2018) |
|
Consulting and
assisting searching service |
UGME |
Personal
librarian program |
USA |
2013-18 |
2018 |
(Gillum et
al., 2018) |
|
Real-time
clinical searching service |
CE |
Clinical
rounds |
USA |
2014-19 |
2019 |
(Gibbons &
Werner, 2019) |
a Residency
Education, b Under-Graduated Medical Education, c
Continuing Professional Education,
d Clinical
Education
Data Analysis
In
this study, we used a narrative review technique for bringing together findings
of the different studies and accomplishing the review. Narrative analysis with
tabular accompaniment is a typical analysis technique for reviews (Grant &
Booth, 2009). A narrative review synthesizes the available evidence from
different studies to provide a conclusion from collected literature (Green et
al., 2006). For the analysis of included studies, first we read the articles
carefully. Second, we compared the implementation trends of applied information
services in the educational clinical setting and identified the similarities
and differences between structures of implementation trends. Third, we
extracted the related themes for each similar part of the identified structure
through note-taking. Also, we considered the related themes for any differences
between applied information services. Finally, we organized the related themes
of similar parts of implementation trends within the comparison tables.
Results
Implementation
of a program was defined as developing performing procedures for planned tasks
and achieving determined objectives (National
Minority AIDS Council, 2015). In this regard, we tried to
highlight typical characteristics of implementation trends in EBEIS which were
common amongst included studies. After the analysis and comparison of studies,
we recognized five oft-mentioned elements of information services
implementation trends. In addition, for a better understanding of the
implementation process of information services, we summarized the program
development process and practical effects of information services.
Program Development of Information Services
Program
development has a multi-step process. The main elements of the program
development process are required resources for program implementation, program
designing, and predefined measures for determining outputs of the program (National
Minority AIDS Council, 2015). We determined two elements of
program development by comparing the findings of the included studies.
Prerequisites of Programs
One
of the prerequisites of using EBEIS is understanding EBM principles. It is
essential to ask an evidence based question to receive a relevant response from
the information service (Aitken et al.,
2011; Brian et al., 2018). It is
important to have a librarian present at the point of teaching when the cases
are presented. It helps the librarian more quickly and effectively respond to
the learners’ queries (Aitken et al.,
2011; Blake et al., 2018; Gibbons & Werner, 2019; Herrmann et al., 2017; Yaeger
& Kelly, 2014). Other
prerequisites for an effective information service are speed of Internet
connection and access to evidence based databases. Providing appropriate
evidence based information on an educational-clinical question strongly depends
on the accessibility of information sources like databases (Santos &
Mariano, 2014). In this
regard, the availability of infrastructures like a reference-tracker or data
repository which deposits data like educational-clinical questions/answers,
frequency of responded/non-responded questions, and common clinical patient
problems is essential. Deposits of interacted data can be used for subsequent
referencing and establishing a database of evidence based educational
information for high prevalence clinical disorders (Gillum et al.,
2018).
Process of Designing
If
an information service is intended to support the evidence based needs of a
curriculum, the librarian should consider the structure and needed resources of
the curriculum in the design process (Neves &
Dooley, 2011). In this
regard, surveying the information needs of intended users helped to design the
most appropriate services (Zeblisky et
al., 2015). The diversity
of access channels to information services is an essential factor in the design
process. Access via multiple communication channels like email, web, social
networks, or face-to-face communication facilitates the use of information
services for busy clinicians (Brian et al.,
2018).
Implementation Trends of EBEIS
Schedule and Type of Access to Information Services
The
schedule of implementing information services strongly depended on the volume
of assigned tasks that the librarian had to do alongside the duties of
information services. In addition, information services which used
telecommunications channels like phone or email (Brian et al.,
2018; Gillum et al., 2018; Herrmann et al., 2017; Santos & Mariano, 2014; Weaver,
2011) could provide
services during a wider span of time (Table 3).
In
the included studies, information services were implemented in different levels
of medical education from undergraduate to postgraduate degree programs. In
undergraduate medical education, medical students receive the knowledge and
skills needed to be a junior doctor. Then, the junior doctor receives more
training, especially via clinical education, to gain experience, develop skills
for patient care, and prepare for entrance into residency education. This
period is considered the internship. Residency education is a period of
training to educate competent clinicians in a specific medical specialty such
as internal medicine. Internship and residency programs are the two stages of
postgraduate medical education. Clinical education provides an opportunity for
the trainees to acquire practical skills by rotating between clinical
departments of a hospital. Clinical education is an essential part of
postgraduate training (Weggemans et al., 2017; Wijnen-Meijer et al., 2013). In addition, the final stage
of medical education is continuing professional education (CPE), which promotes
lifelong learning for clinicians within their clinical settings. CPE supports
clinical skill development of medical doctors and enhances the outcomes of
patient treatment (Bennett et al., 2000). CPE programs are delivered via
different methods such as rounds, workshops, seminars, conferences, online
learning, telemedicine, and other methods.
Medical
trainees at the undergraduate and graduate levels receive clinical education in
the teaching setting of morning reports and rounds. Morning report is a
case-based meeting where medical students and their educators discuss a
clinical case related to a patient recently admitted to the teaching hospital
(Amin et al., 2000). Rounds or ward rounds are held beside the patient’s bed
and consist of medical educators and students that listen to the patient and
discuss the case of disease presented (O'Hare,
2008).
Table
3
Schedule/Access
to Information Services
|
Setting |
Type of
education |
Schedule of
implementation |
Type of access |
|
Morning
report/ rounds/ team conference (Aitken et
al., 2011) |
REa |
10-12
hours per week |
Face-to-face |
|
Patient
rounds (Yaeger &
Kelly, 2014) |
RE |
Once
per week |
Face-to-face |
|
Morning
rounds (Santos &
Mariano, 2014) |
CPEb |
Every
working days |
Face-to-face/email/
phone |
|
Morning
rounds (Santos &
Mariano, 2014) |
CPE |
24
hours/ all days of week |
Phone/email |
|
Morning
report (Weaver, 2011) |
RE |
5
days a week |
Face-to-face
/ email |
|
EBM
conference (Zeblisky et
al., 2015) |
RE |
Once
per month |
Face-to-face |
|
Patient-family
centered rounds (Herrmann et
al., 2017) |
CEc |
Not
mentioned |
Face-to-face/
email |
|
Clinical
rounds (Gibbons &
Werner, 2019) |
CE |
Once
a week |
Face-to-face |
|
Inpatient
rounds (Brian et al.,
2018) |
CE |
Between
3 to 5 days a week |
Face-to-face/
email |
|
Personal
librarian program (Gillum et
al., 2018) |
UGMEd |
When
the users needed |
Face-to-face/
email |
a
Residency
Education, b Continuing Professional Education, c
Clinical Education, d Under-Graduated Medical Education
Methods of Receiving Educational-Clinical Questions
In
most of the implementation trends for EBEIS, there is a preference for the
presence of a librarian in educational-clinical meetings such as rounds,
morning reports, and EBM conferences (Aitken et al.,
2011; Brian et al., 2018; Gibbons & Werner, 2019; Herrmann et al., 2017;
Santos & Mariano, 2014; Weaver, 2011; Yaeger & Kelly, 2014; Zeblisky et
al., 2015). However, some
of the information services were provided only virtual, with online chatting as
a predefined connection channel between librarians and users. Also, users were
able to submit their feedback on the quality of information services via a text
box on the web (Neves &
Dooley, 2011). Another
channel that was provided for receiving educational-clinical queries was an
online submission form. Receiving queries online made access to information
services easier (Brian et al.,
2018).
Types of Delivery of Information Services
The
most prevalent type of EBEIS was mediated searching and document delivery based
on educational-clinical queries (Aitken et al.,
2011; Brian et al., 2018; Gibbons & Werner, 2019; Herrmann et al., 2017;
Santos & Mariano, 2014; Weaver, 2011; Yaeger & Kelly, 2014), consulting
services for how to formulate a question, and assistance searching the evidence
(Blake et al.,
2018; Gillum et al., 2018; Herrmann et al., 2017; Santos & Mariano, 2014; Zeblisky
et al., 2015). With mediated
searching, the librarian received queries, searched appropriate databases, and
delivered relevant evidence to the student.
Table
4
Evidence
Based Outputs of Information Services
|
Reference
number |
Case
presentation |
Controlled
vocabulary |
Key
words |
Applied
search strategy |
Search
results |
Full-text
of search results |
Abstract
of search results |
Type
of education |
|
(Yaeger &
Kelly, 2014) |
-
a |
+
b |
+ |
+ |
+ |
- |
- |
Residency
education |
|
(Santos &
Mariano, 2014) |
-
|
- |
- |
- |
- |
+ |
+ |
Continuing
professional education |
|
(Weaver, 2011) |
+ |
- |
- |
- |
+ |
- |
- |
Residency
education |
|
(Herrmann et
al., 2017) |
- |
- |
- |
- |
- |
- |
+ |
Clinical
education |
|
(Brian et al.,
2018) |
- |
- |
- |
- |
- |
+ |
- |
Clinical
education |
|
(Blake et al.,
2018) |
+ |
- |
- |
- |
- |
- |
- |
Under-graduate
medical education |
a not-provided, b
provided
Time of Responding to Queries
The
time that it took a librarian to respond to the educational-clinical questions
influenced the intended learning of trainees. Some of the information services
were designed to provide the needed evidence based information at the
educational session itself or on the same day (Aitken et al.,
2011; Brian et al., 2018; Gibbons & Werner, 2019; Yaeger & Kelly, 2014). In other
studies, the authors did not mention time expectations for receiving answers (Herrmann et
al., 2017; Santos & Mariano, 2014; Weaver, 2011). With
information services that provided online access to questions and answers,
librarians responded to queries in one to three days (Brian et al.,
2018).
Providing Evidence Based Outputs
The
preparation of evidence based outputs for evidence requests is an essential
part of an educational information service. Evidence based output is a document
of what a librarian has done to fulfill an evidence request. The evidence based
output consists of three distinct parts: a) the clinical case presentation of
the patient, b) a record of what keywords and search strategies were used for
retrieving evidence, and c) the retrieved search results, which may include the
abstracts and full text. Each information service examined presented at least
one aspect of the outputs, but a service with all these outputs better supports
the educational needs. The purpose of preparing outputs is to provide a
documented record for what librarians do, thereby helping trainees and
educators learn to better perform their own search for retrieving needed
evidence. Preparing an evidence based output for each request of clinical
evidence is time-consuming for the librarian, but educators and learners then
have the information documented for further learning and later referrals, as
well as evidence based data to deposit in local evidence based databases for
future educational purposes (see Table 4).
Effects on Trainee Learning
In
the field of medical education, EBEIS enhanced learners’ understanding of
evidence based practice in medicine (Blake et al.,
2018; Brian et al., 2018; Yaeger & Kelly, 2014). After learning
about EBM resources (Blake et al.,
2018; Brian et al., 2018; Gibbons & Werner, 2019), the evidence
retrieval behaviour of medical students shifted to more reliable databases for
finding answers to clinical questions (Aitken et al.,
2011). The evidence
based searching skills of learners were strengthened and learners were able to
formulate more meaningful evidence based searches (Brian et al.,
2018; Herrmann et al., 2017; Zeblisky et al., 2015). In addition,
providing such information services meant learners were supplied up-to-date,
high-quality information more quickly (Brian et al.,
2018; Gibbons & Werner, 2019), and enhanced
the learning process (Gibbons &
Werner, 2019). Another
practical effect of EBEIS was saving time for learners in finding
needed evidence (Herrmann et
al., 2017).
Discussion
According
to an analysis of the included studies, EBEIS have been implemented in
different types of teaching-related units (e.g., teaching hospitals), and in
varied target settings (e.g., clinical rounds). In all educational settings,
there is a need for learners to access evidence. EBEIS were flexible in
servicing different needs within their predetermined teaching programs. In this
regard, information services can be implemented in different educational
settings with diverse types of access and schedules of service delivery.
Consequently, changes in curricula and teaching programs that produce new
information needs can be met with reciprocal revisions in the implementation
plan of the information services.
It
is noteworthy that some of the studied information services had unique
procedures in their implementation, which were not executed in the other
information services, and therefore were not categorized into identified
characteristics as a part of this study. Yaeger and Kelly (2014) stated in
their study that a pre-prepared summary of the patient’s clinical situation and
current clinical management was provided for the librarian ahead of clinical
meetings. This procedure helped the librarian to present in the meetings with
more confidence, especially for librarians who are new to delivering EBEIS.
In
some circumstances, the librarian taught the trainees EBM principles and
skills, including understanding and creating PICO questions and designing a
search strategy according to the PICO structure, to help accomplish one of the
prerequisites of using EBEIS (Aitken et al., 2011; Zeblisky
et al., 2015). In this regard, librarians in some of the information services
collaborated with teaching teams to prepare educational materials for trainees.
In such situations, librarians working in the clinical environment could
provide more applicable materials than those excluded from clinical situations
(Blake et al., 2018). In this regard, Safdari et al.
(2018) found the types of educational roles and activities of health care
librarians in teaching information literacy skills and evidence based practice
principles to medical students, educators, and clinicians, especially in the
location of clinics or via online training. Such educational activities
included developing interactive online tutorials, developing video
instructions, and co-teaching in medical faculties. Safadari
et al. identified librarian participation methods in educational programs that
can be considered in the development of EBEIS.
Another
unique procedure which supported student learning was assigning a group of trainees
with a set number to each librarian. The librarian monitored the students’
skill learning according to pre-determined learning objectives, and
reciprocally, each student knew which librarian to contact when they
encountered a learning problem (Gillum et al., 2018).
Figure
2 presents a schematic diagram of identified characteristics of information
services within the sequence of program implementation. Also, we included
uncategorized characteristics of information services in the diagram, described in the previous paragraphs.
The
main limitation of this study was differentiating between evidence based
information services which were designed for clinical practice, medical
education, or both simultaneously. In this respect, we tried to include studies
which explained the implementation of an information service for supporting
evidence for any type of educational procedure.
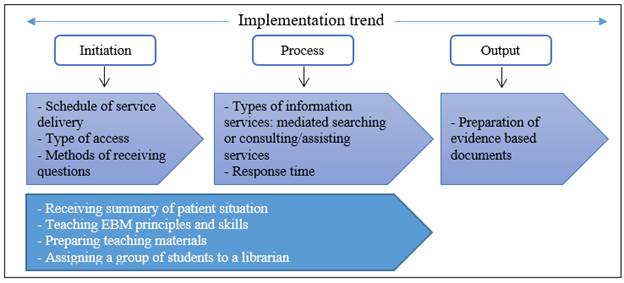
Figure
2
Schematic
diagram of implementation characteristics of information services.
Conclusion
We
conducted this study to identify the structure of the implementation process of
information services which supported evidence based medical education. After
conducting search strategies in target databases and employing
inclusion/exclusion criteria, we selected and analyzed 11 articles. Information
services which were studied in this review supported empirical knowledge for
evidence based medical education at different levels of training and
facilitated evidence based change in educational approaches. The summarized
trend of implementing EBEIS consisted of:
(1)
schedule and type of access;
(2)
methods for receiving questions;
(3)
information service types;
(4)
response time; and
(5)
preparation of evidence based outputs.
On
the basis of the implementation trends of information services being studied,
an applicable EBEIS based on the needs of each educational level can be
designed.
According
to the findings of the current review, we propose the following practical
recommendations. First, a needs assessment of predefined users is a necessary
prerequisite before designing a practical EBEIS. Based on the characteristics
of stakeholders of information services, librarians can benefit from various
needs assessment techniques. The characteristics and needs of stakeholders
should determine the appropriate assessment technique that results in the most
useful data. Second, each educational level needs to have a
specifically-designed information service separately. Third, mediated searching
can be used for undergraduate levels and consulting information services can be
used for graduate or professional levels. Fourth, types of data needed in the
evidence based outputs depend on the needs of intended users. Finally, more
detailed evidence based outputs will fulfill more educational needs in the
future.
It
is also plausible to suggest future studies to compare the structure of
evidence based information services which support clinical practice with
information services that were developed for medical education, in order to
identify additional characteristics of implementation trends of evidence based
information services.
Acknowledgements
This
study is part of a Ph.D. thesis supported by the Iran University of Medical
Sciences under Grant No. IR.IUMS.FMD.REC_1396.9381623003.
Author Contributions
Sedigheh Khani: Conceptualization, Data curation, Methodology,
Visualization, Writing – original draft Sirous
Panahi: Conceptualization, Data curation, Methodology, Writing – review
& editing Ali Pirsalehi: Conceptualization,
Writing – review & editing Ata Pourabbasi: Conceptualization,
Writing – review & editing
References
Aitken, E. M.,
Powelson, S. E., Reaume, R. D., & Ghali,
W. A. (2011). Involving clinical librarians at the point of care: Results of a
controlled intervention. Academic
Medicine, 86(12), 1508-1512. https://doi.org/10.1097/ACM.0b013e31823595cd
Amin, Z.,
Guajardo, J., Wisniewski, W., Bordage, G., Tekian, A., & Niederman, L. G. (2000). Morning report:
Focus and methods over the past three decades. Academic Medicine, 75(10),
S1-5. https://doi.org/10.1097/00001888-200010001-00002
Bennett, N. L.,
Davis, D. A., Easterling, W. E., Friedmann, P., Green, J. S., Koeppen, B. M., Mazmanian, P. E., & Waxman, H. S.
(2000). Continuing medical education: A new vision of the professional
development of physicians. Academic Medicine, 75(12), 1167–1172. https://doi.org/10.1097/00001888-200012000-00007
Blake,
L., Yang, F. M., Brandon, H., Wilson, B., & Page, R. (2018). A clinical
librarian embedded in medical education: Patient-centered encounters for
preclinical medical students. Medical
Reference Services Quarterly, 37(1), 19-30. https://doi.org/10.1080/02763869.2018.1404384
Brian,
R., Orlov,
N., Werner, D., Martin, S. K., Arora, V. M., & Alkureishi,
M. (2018). Evaluating the impact of clinical librarians on clinical questions
during inpatient rounds. Journal of the
Medical Library Association, 106(2), 175-183. https://doi.org/10.5195/jmla.2018.254
Burns, P.
B., Rohrich, R. J., & Chung, K. C. (2011).
The levels of evidence and their role in evidence-based medicine.
Plastic and Reconstructive Surgery, 128(1), 305-310. https://doi.org/10.1097/PRS.0b013e318219c171
Chessare,
J. B. (1996). Evidence-based medical education: The missing variable in the
quality improvement equation. The Joint
Commission Journal on Quality Improvement, 22(4), 289-291. https://doi.org/10.1016/s1070-3241(16)30232-2
Davies,
P. (1999). What is evidence-based education? British Journal of Educational Studies, 47(2), 108-121. https://doi.org/10.1111/1467-8527.00106
Davies,
S., Herbert, P., Wales, A., Ritchie, K., Wilson, S., Dobie, L., & Thain,
A. (2017). Knowledge into action - Supporting the implementation of evidence
into practice in Scotland. Health
Information and Libraries Journal, 34(1), 74-85. https://doi.org/10.1111/hir.12159
Djulbegovic,
B., & Guyatt, G. H. (2017). Progress in evidence-based
medicine: A quarter century on. Lancet,
390(10092), 415-423. https://doi.org/10.1016/s0140-6736(16)31592-6
EBSCO.
(n.d.-a). Information services. In Library, Information Science & Technology
Abstracts Thesaurus. Retrieved March 15, 2021, from http://www.libraryresearch.com/
EBSCO.
(n.d.-b). Information services in education. In Library, Information Science
& Technology Abstracts Thesaurus. Retrieved March 15 2021, from http://www.libraryresearch.com/
Emami,
S. A. H., Khankeh, H., Karbasi
Motlagh, M., Zarghi, N.,
& Shirazi, M. (2019). Exploring experience of Iranian medical sciences
educators about Best Evidence Medical Education: A content analysis. Journal of Education and Health Promotion, 8,
247-252. https://doi.org/10.4103/jehp.jehp_428_19
Fennessy,
G. (2001). Knowledge management in evidence-based healthcare: Issues raised
when specialist information services search for the evidence. Health Informatics Journal, 7(1), 4-7. https://doi.org/10.1177/146045820100700102
Gibbons,
P., & Werner, D. A. (2019). Embedded clinical librarianship: Bringing
medical reference services bedside. Public
Services Quarterly, 15(2), 169-175. https://doi.org/10.1080/15228959.2019.1583153
Gillum,
S., Williams, N., Herring, P., Walton, D., & Dexter, N. (2018). Encouraging
engagement with students and integrating librarians into the curriculum through
a personal librarian program. Medical
Reference Services Quarterly, 37(3), 266-275. https://doi.org/10.1080/02763869.2018.1477710
Grant,
M. J., & Booth A. (2009). A typology of reviews: An analysis of 14 review
types and associated methodologies. Health
Information and Libraries Journal, 26, 91-108. https://doi.org/10.1111/j.1471-1842.2009.00848.x
Green,
B. N., Johnson, C. D., & Adams A. (2006). Writing narrative literature
reviews for peer-reviewed journals: Secrets of the trade. Journal of
Chiropractic Medicine, 5(3), 101-117. https://doi.org/10.1016/S0899-3467(07)60142-6
Guyatt,
G., Cairns, J., Churchill, D., Cook, D., Haynes, B., Hirsh, J., Irvine, J.,
Levine, M., Levine, M., Nishikawa, J., Sackett, D., Brill-Edwards, P.,
Gerstein, H., Gibson, J., Jaeschke, R., Kerigan, A., Neville, A., Panju,
A., Detsky, A., … Enkin, M.
(1992). Evidence-based medicine: A new approach to teaching the practice of
medicine. Journal of the American Medical Association, 268(17),
2420-2425. https://doi.org/10.1001/jama.1992.03490170092032
Haig,
A., & Dozier, M. (2003a). BEME Guide No 3: Systematic searching for
evidence in medical education—Pt. 1: Sources of information. Medical Teacher, 25(4), 352-363. https://doi.org/10.1080/0142159031000136815
Haig,
A., & Dozier, M. (2003b). BEME Guide No. 3: Systematic searching for
evidence in medical education—Pt. 2: Constructing searches. Medical Teacher, 25(5), 463-484. https://doi.org/10.1080/01421590310001608667
Harden,
R. M., Grant, J., Buckley, G., & Hart, I. R. (2000). Best evidence medical
education. Advances in Health Sciences
Education: Theory and Practice, 5(1), 71-90. https://doi.org/10.1023/a:1009896431203
Hart,
I. R., & Harden, R. M. (2000). Best Evidence Medical Education (BEME): A
plan for action. Medical Teacher, 22(2),
131-135. https://doi.org/10.1080/01421590078535
Herrmann,
L. E., Winer, J. C., Kern, J., Keller, S., & Pavuluri,
P. (2017). Integrating a clinical librarian to increase trainee application of
evidence-based medicine on patient family-centered rounds. Academic Pediatrics, 17(3), 339-341. https://doi.org/10.1016/j.acap.2016.11.005
Holland,
J., & Haynes, R. B. (2005). McMaster
Premium Literature Service (PLUS): An evidence-based medicine information
service delivered on the Web. AMIA ... Annual Symposium proceedings /
AMIA Symposium, 2005, 340-344. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1560593
Jordan,
Z., & Porritt, K. (2004). Evidence-based health information provision:
Development of an online consumer 'request for information' service. Worldviews on Evidence-Based Nursing, 1(4),
237-240. https://doi.org/10.1111/j.1524-475X.2004.04065.x
Liberati,
A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., AIoannidis, J.
P., Clarke, M., Devereaux, P. J., Kleijnen, J., &
Moher, D. (2009). The PRISMA statement for reporting systematic reviews and
meta-analyses of studies that evaluate healthcare interventions: Explanation
and elaboration. British Medical Journal, 339, b2700. https://doi.org/10.1136/bmj.b2700
McGowan,
J., Hogg, W., Rader, T., Salzwedel,
D., Worster, D., Cogo, E.,
& Rowan, M. (2010). A rapid evidence-based service by librarians provided
information to answer primary care clinical questions. Health Information and Libraries Journal, 27(1), 11-21. https://doi.org/10.1111/j.1471-1842.2009.00861.x
National
Minority AIDS Council. (2015). Program
development. http://www.nmac.org/wp-content/uploads/2015/04/Program-Development.pdf
Neves,
K., & Dooley, S. J. (2011). Using LibGuides to offer library service to
undergraduate medical students based on the case-oriented problem solving
curriculum model. Journal of the Medical
Library Association, 99(1), 94-97. https://doi.org/10.3163/1536-5050.99.1.017
O'Hare, J. A.
(2008). Anatomy of the ward round. European Journal of Internal Medicine, 19(5),
309-313. https://doi.org/10.1016/j.ejim.2007.09.016
Onyura,
B., Légaré, F., Baker, L., Reeves, S., Rosenfield,
J., Kitto, S., Hodges B., Silver I., Curran V., Armson H., & Leslie, K. (2015). Affordances of
knowledge translation in medical education: A qualitative exploration of empirical
knowledge use among medical educators. Academic
Medicine, 90(4), 518-524. https://doi.org/10.1097/acm.0000000000000590
Poirier,
T., & Behnen,
E. (2014). Where and how to search for evidence in the education literature:
The WHEEL. American Journal of
Pharmaceutical Education, 78(4), 70-77. https://doi.org/10.5688/ajpe78470
Reed,
D., Price, E. G., Windish,
D. M., Wright, S. M., Gozu, A., Hsu, E. B., Beach M.
C., Kern D., & Bass, E. B. (2005). Challenges in systematic reviews of
educational intervention studies. Annals
of Internal Medicine, 142(12 Pt. 2), 1080-1089. https://doi.org/10.7326/0003-4819-142-12_part_2-200506211-00008
Sackett, D. L.,
Rosenberg, W. M., Gray, J. A., Haynes, R. B. & Richardson, W. S. (1996).
Evidence based medicine: What it is and what it isn't. British Medical
Journal, 312(7023), 71-72. https://doi.org/10.1136/bmj.312.7023.71
Safdari, R., Ehtesham, H., & Bahadori, L.
(2018). Highlighting a valuable dimension in health care librarianship: A
systematic review. Medical Journal of the Islamic Republic of Iran, 32,
1-7. https://doi.org/10.14196/mjiri.32.42
Sandars,
J., & Patel, R. (2015). It's OK for you but maybe not for me: The challenge
of putting medical education research findings and evidence into practice. Education for Primary Care, 26(5),
289-292. https://doi.org/10.1080/14739879.2015.1079008
Santos,
M. A. A., & Mariano, G. S. L. (2014). Information professional at the point
of care: Clinical librarian service in neurocritical care. Journal of Philippine Librarianship, 34, 61-69. https://journals.upd.edu.ph/index.php/jpl/article/view/4585
Shortell,
S. M., Rundall, T. G., & Hsu, J. (2007).
Improving patient care by linking evidence-based medicine and evidence-based
management. JAMA, 298(6), 673-676. https://doi.org/10.1001/jama.298.6.673
Sur,
R. L., & Dahm,
P. (2011). History of evidence-based medicine. Indian Journal of Urology: IJU: Journal of the Urological Society of
India, 27(4), 487-489. https://doi.org/10.4103/0970-1591.91438
Suttle,
C. M., Challinor,
K. L., Thompson, R. E., Pesudovs, K., Togher, L., Chiavaroli, N., Lee
A., Junghans B., Stapleton F., Watt K., & Jalbert, I. (2015). Attitudes and barriers to
evidence-based practice in optometry educators. Optometry and Vision Science, 92(4), 514-523. https://doi.org/10.1097/opx.0000000000000550
Thomas,
A., Gruppen, L. D., Vleuten, C. V. D., Chilingaryan,
G., Amari, F., & Steinert, Y. (2019). Use of evidence in health professions
education: Attitudes, practices, barriers and supports. Medical Teacher, 41(9), 1012-1022. https://doi.org/10.1080/0142159x.2019.1605161
Weaver,
D. (2011). Enhancing resident morning report with “Daily Learning Packages”. Medical Reference Services Quarterly, 30(4),
402-410. https://doi.org/10.1080/02763869.2011.609077
Weggemans, M. M., Dijk,
B, V., Dooijeweert, B. V., Veenendaal,
A. G., & Cate, O. T. (2017). The postgraduate medical education pathway: An
international comparison. GMS Journal for Medical Education, 34(5),
1-16. https://doi.org/10.3205/zma001140
Wijnen-Meijer, M., Burdick,
W., Alofs, L., Burgers, C., & Cate, O. T. (2013). Stages and transitions in
medical education around the world: Clarifying structures and
terminology. Medical Teacher, 35(4), 301-307. https://doi.org/10.3109/0142159X.2012.746449
Yaeger,
L. H., & Kelly, B. (2014). Evidence-based medicine: Medical librarians
providing evidence at the point of care. Missouri
Medicine, 111(5), 413-415. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6172079
Zeblisky,
K., Birr, R. A., & Guerrero, A. M. S. (2015). Effecting change in an
evidence-based medicine curriculum: Librarians' role in a pediatric residency
program. Medical Reference Services
Quarterly, 34(3), 370-381. https://doi.org/10.1080/02763869.2015.1052702