When an individual has cancer, or any number of other diseases, early detection can make a huge difference in the outcome. A research team led by the University of Notre Dame is working to cut the test time for disease biomarkers. The new timeline — 30 minutes instead of 13 hours — uses even smaller sample sizes to offer a new liquid biopsy option.
The difference is an integrated microfluidics platform developed at Notre Dame that uses extracellular vesicles (EVs) containing microRNAs (miRNAs) as biomarkers for early-stage disease diagnosis.
“Extracellular vesicles contribute to intercellular communication, especially during specific cellular processes such as coagulation or immune responses,” said Hsueh-Chia Chang, co-lead of the study and Bayer Professor of Chemical and Biomolecular Engineering at Notre Dame. “More importantly, we are just now learning that EVs and the microRNA they carry also play a role in disease proliferation. If we can detect them accurately, quickly and cost-effectively, they could very well be the key to early cancer detection.”
Cells secrete EVs, which are easily isolated in bodily fluids such as blood, saliva and even breastmilk.
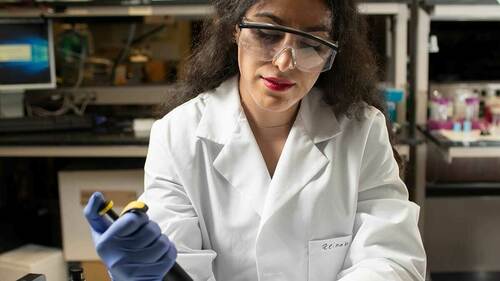
Chang’s team developed a viable screening tool that significantly improves the inefficiencies of more conventional methods of EV-miRNA analysis.
“What we’ve developed is essentially a microfluidic chip that takes a small amount of blood plasma and analyzes it for a target EV microRNA in about 30 minutes,” said David Go, Rooney Family Associate Professor of Engineering at Notre Dame and a co-lead on the study. “By using a mechanical piezoelectric device to break open the EVs and an electrical device to detect the microRNA, we remove all the inefficiencies associated with purification, extraction and RNA detection using PCR-based approaches — and it’s a lot faster.”
The study, published in Nature Communications Biology, details the screening tool and its performance. The Notre Dame team worked with cancer researchers from the University of Southern California, including Reginald Hill, assistant professor of medicine at the Keck School of Medicine and the Lawrence J. Ellison Institute for Transformative Medicine, and Bangyan Stiles, professor in the USC School of Pharmacy, to test the new device with both human and mouse liver cancer samples, demonstrating its clinical potential.
One of the most exciting aspects of the device is that it can be easily extended for other RNA and DNA biomarkers and potentially even proteins. The Notre Dame team has already started exploring other early-detection challenges such as preeclampsia and pancreatic cancer. As they continue to develop the technology, the team aims to offer the first liquid biopsy diagnostic device that is simple, rapid, user-friendly and capable of detecting biomarkers from clinical samples as early in the disease process as possible.
“Such a device could profoundly change how we approach health care and, more importantly, provide a better quality of life,” Chang said. “We believe we are well on our way.”
Co-authors on the study include Satyajyoti Senapati, research assistant professor of chemical and biomolecular engineering; Zeinab Ramshani, a postdoctoral researcher in chemical and biomolecular engineering; and Chenguang Zhang, engineering graduate student, all at Notre Dame.
The National Institutes of Health, C. Moschetto Discovery Fund and Notre Dame’s Advanced Diagnostics and Therapeutics initiative funded the study in collaboration with the Center for Microfluidics and Medical Diagnostics at Notre Dame and the Harper Cancer Research Institute.
Contact: Jessica Sieff, assistant director of media relations, 574-631-3933, jsieff@nd.edu